- Home
- DescriptionNews
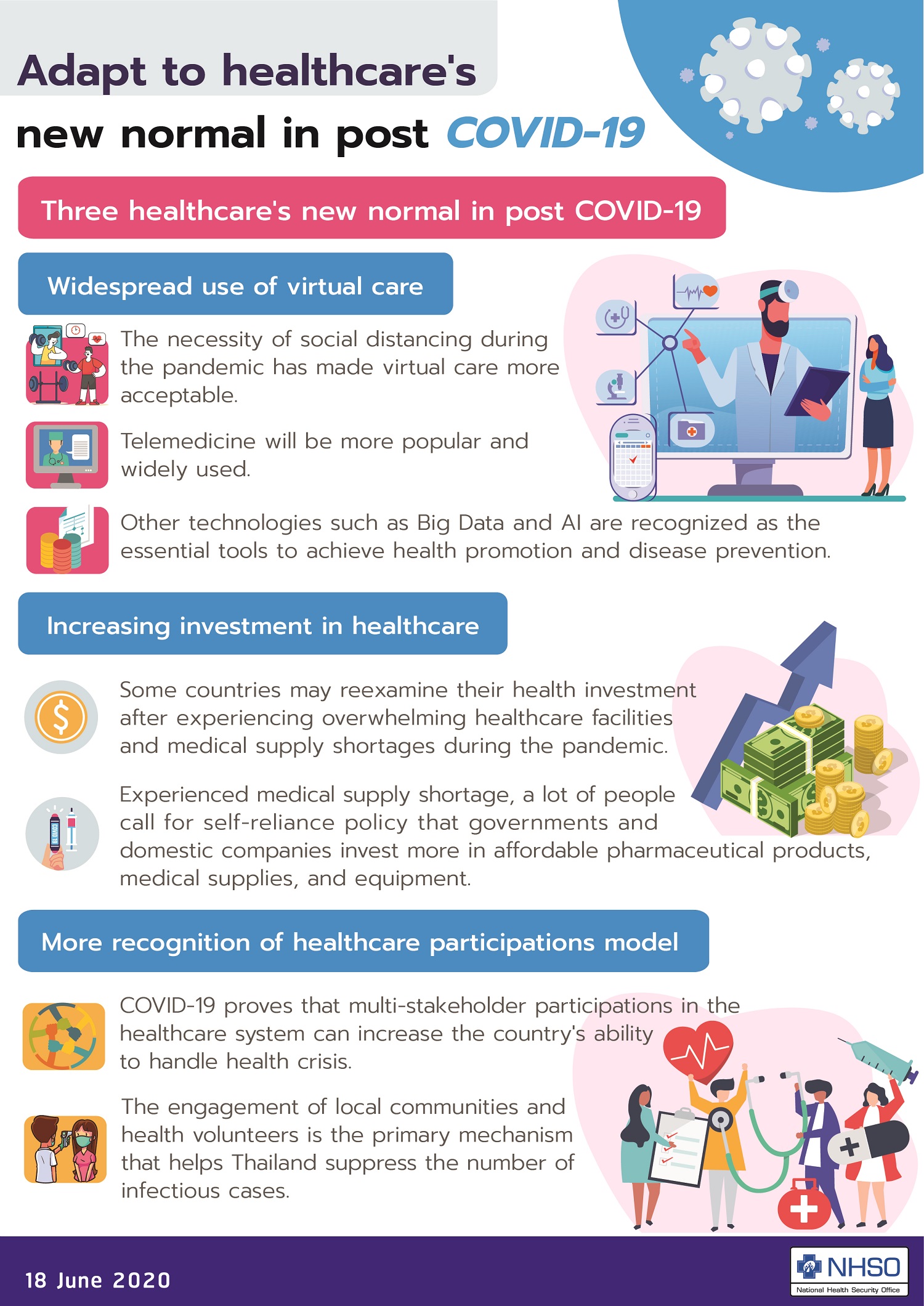
Adapt to healthcare's new normal in post-COVID-19
.jpg)
Prior to the COVID-19 pandemic, the landscape of healthcare was changing by the introduction of new technology. Telemedicine, for example, has facilitated virtual care in many hospitals across the globe. Artificial intelligence and novel medical devices have advanced precision medicine, allowing patients to personalize their care and treatment.
Many experts predict that emerging medical technology will positively influence the healthcare industry—by improving the quality of patient care and saving the lives of millions of people. Some technology, primarily virtual care, has become more acceptable to both physicians and patients while they must stay home to avoid COVID-19 in the past months.
We, as health workers and staff of National Health Security Office (NHSO) which operates Universal Coverage Scheme (UCS) in Thailand, must adapt and act faster to seize an opportunity from quickly developing technology.
We expect to see three major healthcare trends, called "new normal", in the post-COVID-19 period.
First, virtual care will play essential roles in the healthcare system. Many physicians once believed that face-to-face patient care was the only option. The necessity of social distancing during the pandemic has made them see the potential of virtual care, and how to use it for minimizing healthcare costs and maximize the quality of treatment.
For example, some Thai doctors in rural hospitals managed to communicate with COVID-19 patients via Line application's VDO call. Virtual consultation helps reduce the virus exposure risk of health workers and patients' relatives. It also minimizes the use of personal protective equipment, especially the disposable hazmat suits, which was in shortage during the peak of the outbreak.
On the other hands, the pandemic shows that using Big Data can improve the efficiency of emergency response and healthcare services as a whole. In Taiwan, Big Data helps identify the source of disease and trace the people contracting to the confirmed cases, leading to the country's achievement in containing the spread of the virus.
Some hospital operators may learn the advantage of using other technologies—such as logistic dashboards that can effectively monitor, manage and deploy essential resources including hospital beds, drugs, and personal protective equipment.
Second, some countries may reexamine their health investment after experiencing overwhelming healthcare facilities and medical supply shortages during the pandemic.
International organizations such as the World Health Organization and the World Bank have emphasized the benefits of health financing in enhancing emergency response capacity and people's resilience to crises. The Philippines government, for example, promises to put more investment in healthcare facilities and UHC after the outbreak disrupted the country's healthcare system.
Experienced medical supply shortage, a lot of people call for self-reliance policy that governments and domestic companies invest more in affordable pharmaceutical products, medical supplies, and equipment.
Finally, COVID-19 proves that multi-stakeholders participations in the healthcare system—from the state, the private sector, local communities to academia and civil society groups—can increase the country's ability to handle a health crisis.
We've observed a good example in South Korea, of which government and private pharmaceutical companies worked together in inventing the new coronavirus test kits. The country was able to control the outbreak within a month by ramping up testing on the full spectrum of the population.
In Thailand, the engagement of local communities and health volunteers is the primary mechanism that helps us suppress the number of infectious cases. They put consistent efforts in tracing and monitoring suspected cases in their residing area, in collaboration with local administration organizations and hospital operators.
Many local communities lead health promotion and disease prevention programs, by educating their neighbors about the symptoms of COVID-19 and how to protect the communities from the virus.
Their engagement in the healthcare system is a powerful social innovation that strengthens emergency response---a distinctive advantage of Thailand, where reciprocity is valued by society.
NHSO sees the urgent need to involve new technology and social innovation in improving UCS, for the best of patients and Thai people as a whole.
Recently, our board members agree to push forward telemedicine in state hospitals to improve patient care. Currently, only 1% of state hospitals apply telemedicine in their healthcare services. We target to increase the ration to 5% next year by funding telemedicine pilot projects in hospitals across the country.
We will also financially support social innovation in community level, one of which is the collaboration between small-scale pharmacies and state hospitals to deliver drugs and medical supplies to patients.
The idea is simple. Hospital operators will deliver supplies to pharmacies in patients' neighborhoods. Pharmacists will then prescribe drugs to patients accordingly to their health conditions and records retrieved from hospital operators.
Patients can reduce the time and travel expenses to hospitals while reducing the risk from the coronavirus. Patients with non-urgent chronic diseases will likely benefit from the delivery the most. Hospital operators, in the meantime, can reduce the workloads and prioritize emergency cases.
Though COVID-19 forced us in temporary turmoil, it also shows us the opportunities and the possibility to use technology and social innovation for the upgrade of the healthcare system.
The more we adapt quickly, the more patients get better care.
Sakchai Kanjanawatana, MD
Secretary-General of Thailand's National Health Security Office (NHSO)
18 June 2020