Ramathibodi Hospital: Making efforts to grow telehealth services
 The necessity of social distancing and self-isolation rules during the COVID-19 outbreak has forced health providers to adapt their services. This is no exception for Ramathibodi Hospital, a university hospital providing super tertiary care in Bangkok.
The necessity of social distancing and self-isolation rules during the COVID-19 outbreak has forced health providers to adapt their services. This is no exception for Ramathibodi Hospital, a university hospital providing super tertiary care in Bangkok."We must change our way of thinking. Before, we encouraged people to see doctors at our hospital. Now we encourage them to improve health literacy so they'll have abilities to look after their heath at home," said Dr Surasak Leelaudomlipi, Director of Ramathibodi Hospital.
"We've experimented some homecare programs in recent years. The COVID-19 outbreak has pushed us to accelerate our effort."
With more than 2.2 millions of visits a year, Ramathibodi Hospital has initiated homecare services for bedridden patients and home-chemotherapy treatment.
"Our staff have discussed launching a medicine home delivery service for some times. But when COVID-19 hit Bangkok, it took us only two weeks to decide and prepare for it. We launched the service on 1 Apr during the peak of the outbreak," said Dr Surasak.
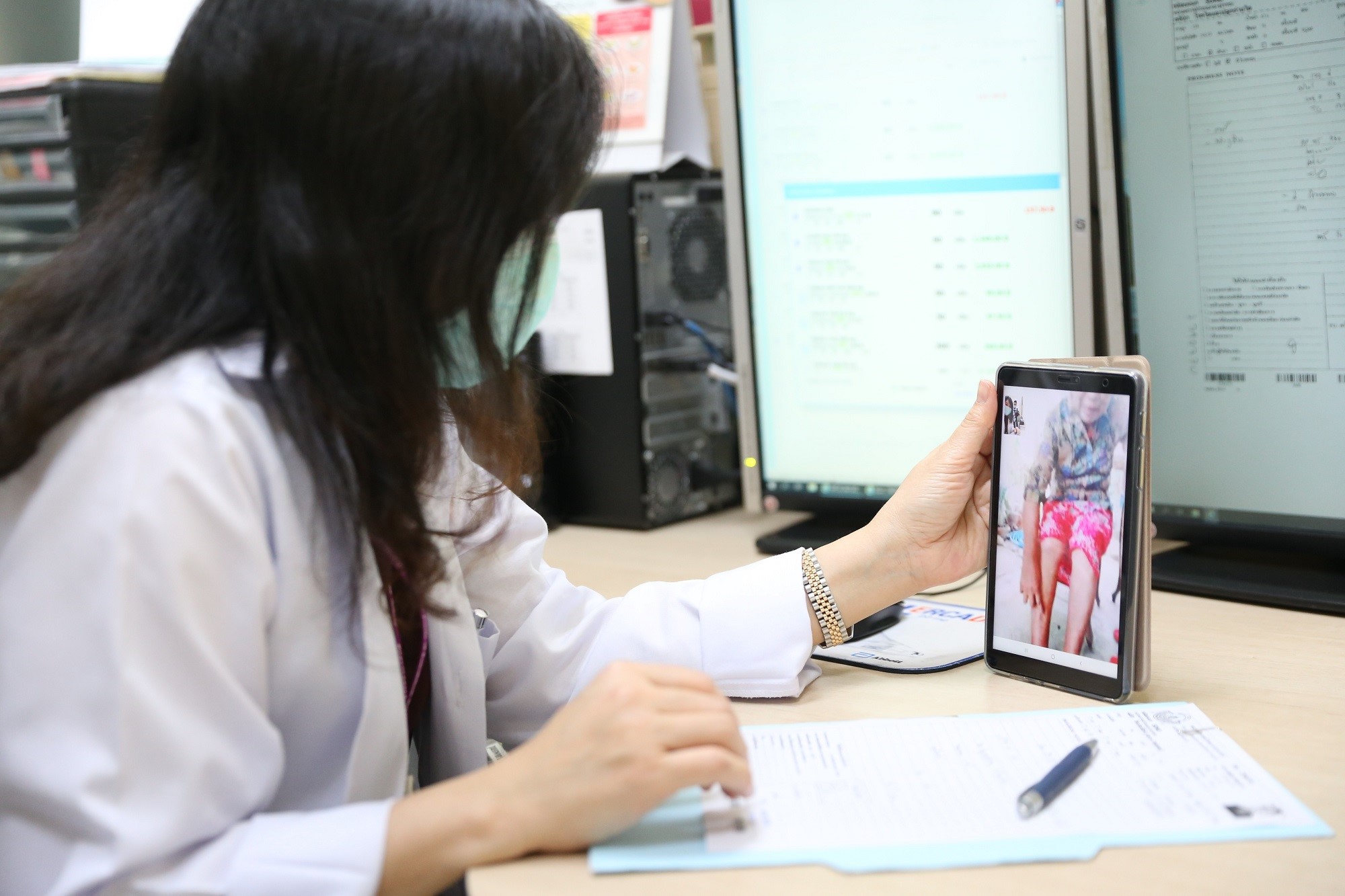
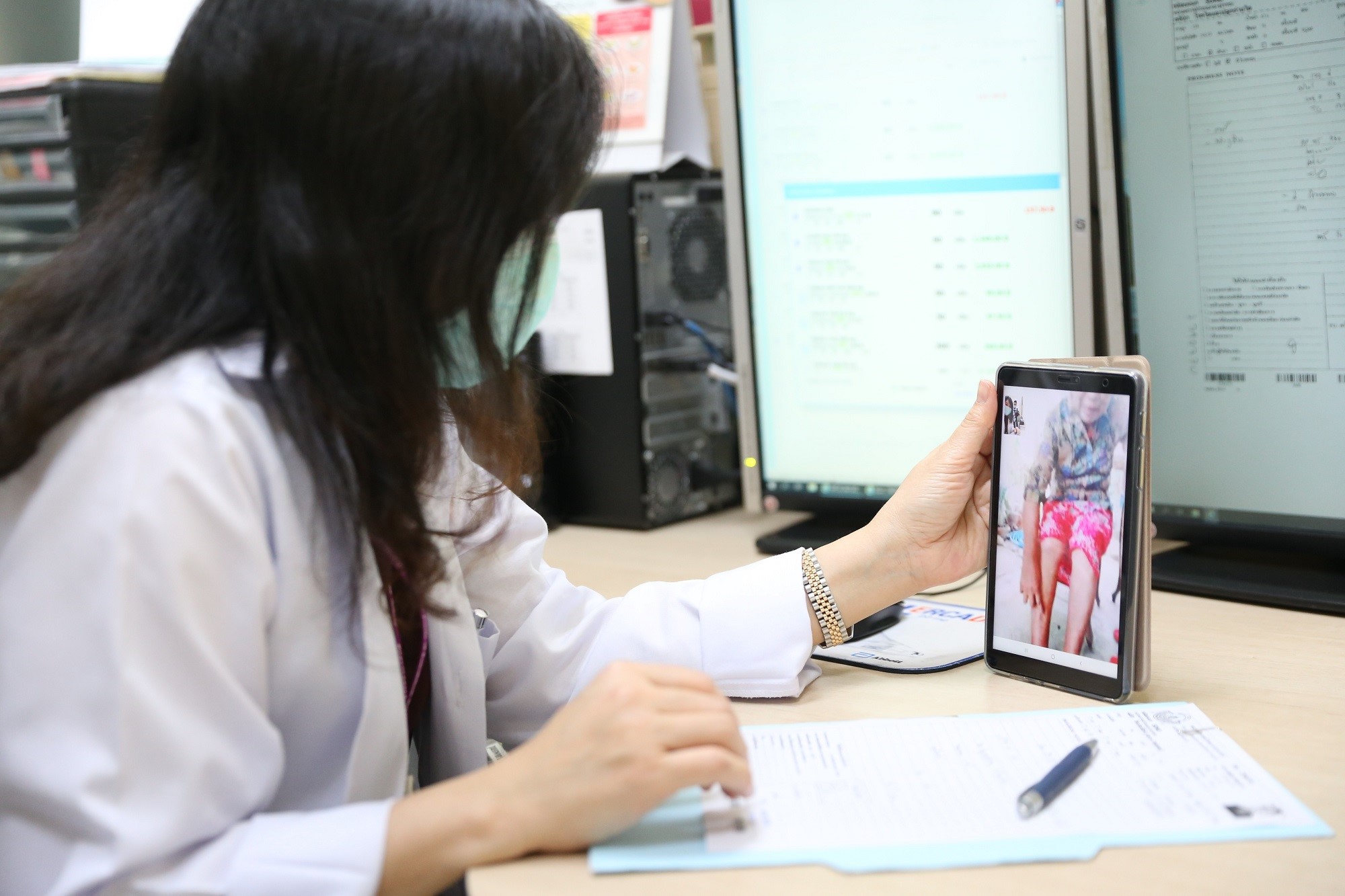
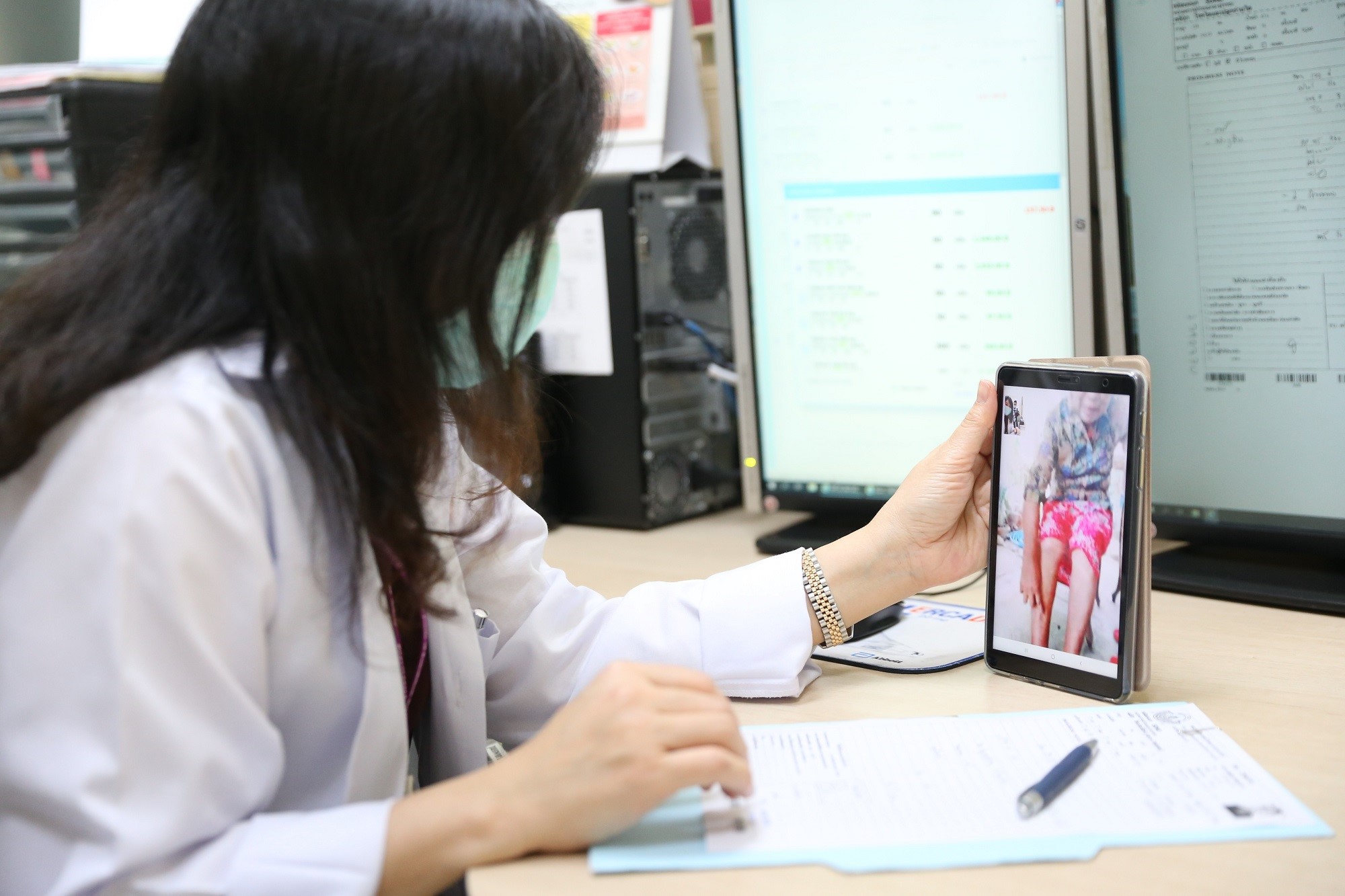
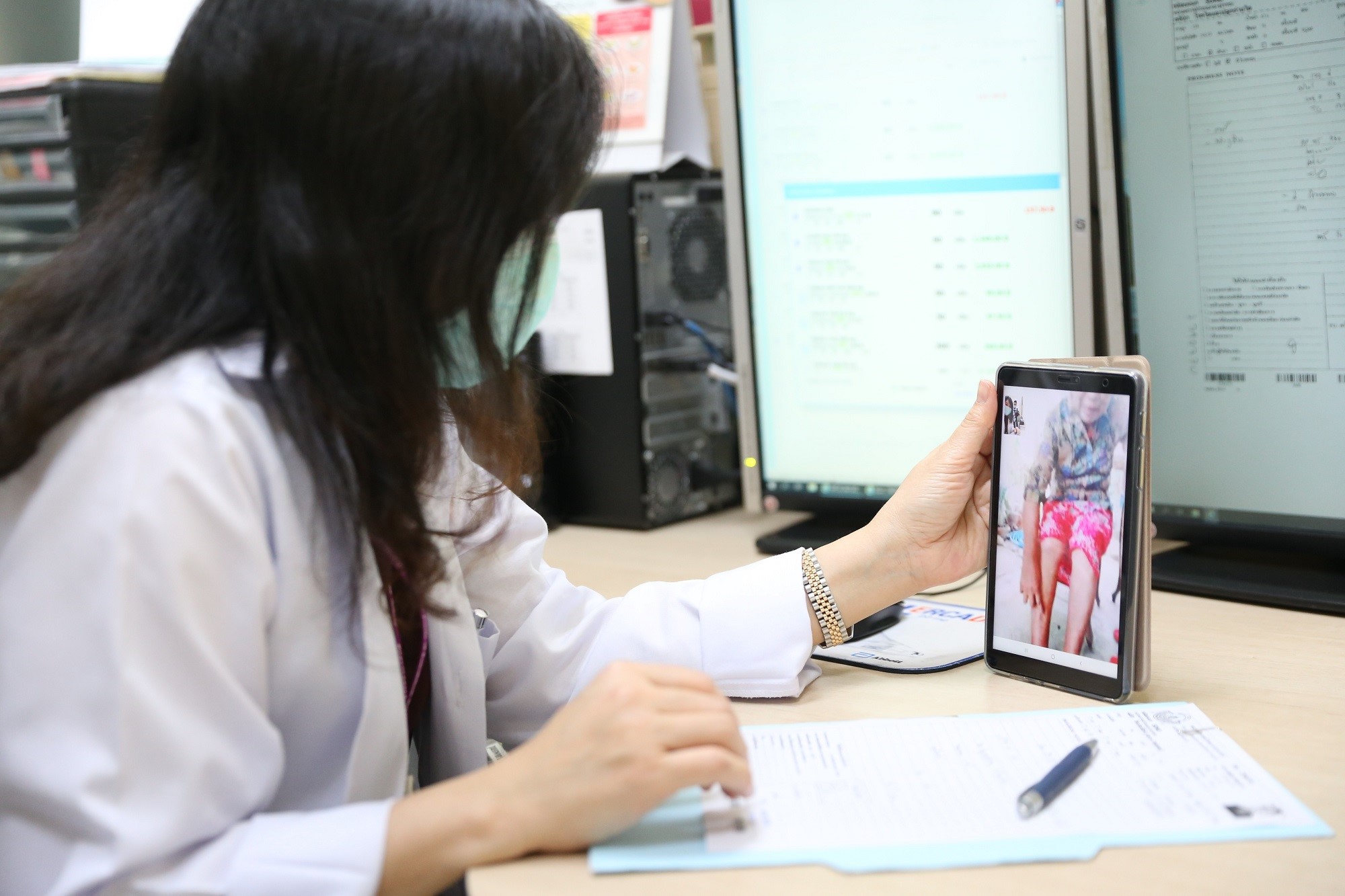
It was about the same time that the hospital staff introduced telemedicine services. Patients can avoid risk from contracting to the coronavirus while traveling to the hospital.
"We needed to redesign our healthcare services and get acceptance from our physicians. This is the real 'new normal' for us," said Dr Atiporn Ingsathit, deputy director of Ramathibodi Hospital.
More than 5,000 patients, or equivalent to 5% of patients requesting medical services in the last two months, have consulted with the hospital staff through telemedicine. Ramathibodi Hospital plans to increase the shares up to 20% in the near future, said Dr Atiporn.
Telemedicine is organized by having physicians who classify patients base on their health conditions. Patients who have stable conditions are classified as 'Green.' Their appointments with doctors can be delayed, or their cases can be referred to community hospitals near their homes.
Patients with stable conditions but require regular consultants are classified as 'Yellow,' which are the main target for telemedicine service. Patients classified as 'Red' are the ones with unstable conditions. They must visit the hospital even though during the pandemic.
After grouping the patients, physicians pass the information to nurses and the medical record department, of which staff will confirm addresses and phone numbers of patients. Then the hospital staff informs patients about their appointment date via SMS.
Patients can consult physicians via phone calls or VDO call applications. After their consultation sessions end, doctors will upload prescriptions of each case into the hospital's database system.
A finance department will then send medical bills to patients via online platforms, and the latter pay through the e-payment system. Finally, the hospital's pharmacists will ship medicine to patients' addresses the next day.
Dr Jadej Thammathacharee, the NHSO deputy secretary-general, said that Ramathibodi Hospital was a role model for health providers that had been proactive and adaptive to the health crisis.
The hospital also provides health services to beneficiaries of Universal Health Coverage, Thai government's healthcare scheme that guarantees healthcare access to more than 49 million Thais.
The NHSO has encouraged health providers at every level, not just the university hospitals like Ramathibodi Hospital, to launch telemedicine and medicine home delivery services. They can reimburse the cost of service from the NHSO.
"We've supported health providers that are adaptive to the new challenges. Their innovation for health services will improve the quality of healthcare delivery," said Dr Jadej.
IN DEPTH
Ramathibodi Hospital: Making efforts to grow telehealth services
 The necessity of social distancing and self-isolation rules during the COVID-19 outbreak has forced health providers to adapt their services. This is no exception for Ramathibodi Hospital, a university hospital providing super tertiary care in Bangkok.
The necessity of social distancing and self-isolation rules during the COVID-19 outbreak has forced health providers to adapt their services. This is no exception for Ramathibodi Hospital, a university hospital providing super tertiary care in Bangkok."We must change our way of thinking. Before, we encouraged people to see doctors at our hospital. Now we encourage them to improve health literacy so they'll have abilities to look after their heath at home," said Dr Surasak Leelaudomlipi, Director of Ramathibodi Hospital.
"We've experimented some homecare programs in recent years. The COVID-19 outbreak has pushed us to accelerate our effort."
With more than 2.2 millions of visits a year, Ramathibodi Hospital has initiated homecare services for bedridden patients and home-chemotherapy treatment.
"Our staff have discussed launching a medicine home delivery service for some times. But when COVID-19 hit Bangkok, it took us only two weeks to decide and prepare for it. We launched the service on 1 Apr during the peak of the outbreak," said Dr Surasak.
It was about the same time that the hospital staff introduced telemedicine services. Patients can avoid risk from contracting to the coronavirus while traveling to the hospital.
"We needed to redesign our healthcare services and get acceptance from our physicians. This is the real 'new normal' for us," said Dr Atiporn Ingsathit, deputy director of Ramathibodi Hospital.
More than 5,000 patients, or equivalent to 5% of patients requesting medical services in the last two months, have consulted with the hospital staff through telemedicine. Ramathibodi Hospital plans to increase the shares up to 20% in the near future, said Dr Atiporn.
Telemedicine is organized by having physicians who classify patients base on their health conditions. Patients who have stable conditions are classified as 'Green.' Their appointments with doctors can be delayed, or their cases can be referred to community hospitals near their homes.
Patients with stable conditions but require regular consultants are classified as 'Yellow,' which are the main target for telemedicine service. Patients classified as 'Red' are the ones with unstable conditions. They must visit the hospital even though during the pandemic.
After grouping the patients, physicians pass the information to nurses and the medical record department, of which staff will confirm addresses and phone numbers of patients. Then the hospital staff informs patients about their appointment date via SMS.
Patients can consult physicians via phone calls or VDO call applications. After their consultation sessions end, doctors will upload prescriptions of each case into the hospital's database system.
A finance department will then send medical bills to patients via online platforms, and the latter pay through the e-payment system. Finally, the hospital's pharmacists will ship medicine to patients' addresses the next day.
Dr Jadej Thammathacharee, the NHSO deputy secretary-general, said that Ramathibodi Hospital was a role model for health providers that had been proactive and adaptive to the health crisis.
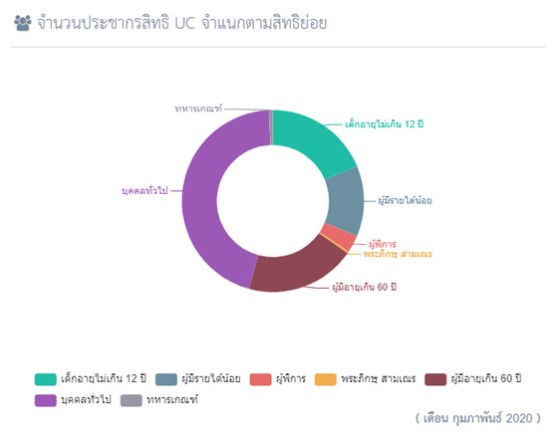
The hospital also provides health services to beneficiaries of Universal Health Coverage, Thai government's healthcare scheme that guarantees healthcare access to more than 49 million Thais.
The NHSO has encouraged health providers at every level, not just the university hospitals like Ramathibodi Hospital, to launch telemedicine and medicine home delivery services. They can reimburse the cost of service from the NHSO.
"We've supported health providers that are adaptive to the new challenges. Their innovation for health services will improve the quality of healthcare delivery," said Dr Jadej.
Events
Ramathibodi Hospital: Making efforts to grow telehealth services
 The necessity of social distancing and self-isolation rules during the COVID-19 outbreak has forced health providers to adapt their services. This is no exception for Ramathibodi Hospital, a university hospital providing super tertiary care in Bangkok.
The necessity of social distancing and self-isolation rules during the COVID-19 outbreak has forced health providers to adapt their services. This is no exception for Ramathibodi Hospital, a university hospital providing super tertiary care in Bangkok."We must change our way of thinking. Before, we encouraged people to see doctors at our hospital. Now we encourage them to improve health literacy so they'll have abilities to look after their heath at home," said Dr Surasak Leelaudomlipi, Director of Ramathibodi Hospital.
"We've experimented some homecare programs in recent years. The COVID-19 outbreak has pushed us to accelerate our effort."
With more than 2.2 millions of visits a year, Ramathibodi Hospital has initiated homecare services for bedridden patients and home-chemotherapy treatment.
"Our staff have discussed launching a medicine home delivery service for some times. But when COVID-19 hit Bangkok, it took us only two weeks to decide and prepare for it. We launched the service on 1 Apr during the peak of the outbreak," said Dr Surasak.
It was about the same time that the hospital staff introduced telemedicine services. Patients can avoid risk from contracting to the coronavirus while traveling to the hospital.
"We needed to redesign our healthcare services and get acceptance from our physicians. This is the real 'new normal' for us," said Dr Atiporn Ingsathit, deputy director of Ramathibodi Hospital.
More than 5,000 patients, or equivalent to 5% of patients requesting medical services in the last two months, have consulted with the hospital staff through telemedicine. Ramathibodi Hospital plans to increase the shares up to 20% in the near future, said Dr Atiporn.
Telemedicine is organized by having physicians who classify patients base on their health conditions. Patients who have stable conditions are classified as 'Green.' Their appointments with doctors can be delayed, or their cases can be referred to community hospitals near their homes.
Patients with stable conditions but require regular consultants are classified as 'Yellow,' which are the main target for telemedicine service. Patients classified as 'Red' are the ones with unstable conditions. They must visit the hospital even though during the pandemic.
After grouping the patients, physicians pass the information to nurses and the medical record department, of which staff will confirm addresses and phone numbers of patients. Then the hospital staff informs patients about their appointment date via SMS.
Patients can consult physicians via phone calls or VDO call applications. After their consultation sessions end, doctors will upload prescriptions of each case into the hospital's database system.
A finance department will then send medical bills to patients via online platforms, and the latter pay through the e-payment system. Finally, the hospital's pharmacists will ship medicine to patients' addresses the next day.
Dr Jadej Thammathacharee, the NHSO deputy secretary-general, said that Ramathibodi Hospital was a role model for health providers that had been proactive and adaptive to the health crisis.
The hospital also provides health services to beneficiaries of Universal Health Coverage, Thai government's healthcare scheme that guarantees healthcare access to more than 49 million Thais.
The NHSO has encouraged health providers at every level, not just the university hospitals like Ramathibodi Hospital, to launch telemedicine and medicine home delivery services. They can reimburse the cost of service from the NHSO.
"We've supported health providers that are adaptive to the new challenges. Their innovation for health services will improve the quality of healthcare delivery," said Dr Jadej.
RESOURCE CENTER
SECRETARY-GENERAL
Ramathibodi Hospital: Making efforts to grow telehealth services
 The necessity of social distancing and self-isolation rules during the COVID-19 outbreak has forced health providers to adapt their services. This is no exception for Ramathibodi Hospital, a university hospital providing super tertiary care in Bangkok.
The necessity of social distancing and self-isolation rules during the COVID-19 outbreak has forced health providers to adapt their services. This is no exception for Ramathibodi Hospital, a university hospital providing super tertiary care in Bangkok."We must change our way of thinking. Before, we encouraged people to see doctors at our hospital. Now we encourage them to improve health literacy so they'll have abilities to look after their heath at home," said Dr Surasak Leelaudomlipi, Director of Ramathibodi Hospital.
"We've experimented some homecare programs in recent years. The COVID-19 outbreak has pushed us to accelerate our effort."
With more than 2.2 millions of visits a year, Ramathibodi Hospital has initiated homecare services for bedridden patients and home-chemotherapy treatment.
"Our staff have discussed launching a medicine home delivery service for some times. But when COVID-19 hit Bangkok, it took us only two weeks to decide and prepare for it. We launched the service on 1 Apr during the peak of the outbreak," said Dr Surasak.
It was about the same time that the hospital staff introduced telemedicine services. Patients can avoid risk from contracting to the coronavirus while traveling to the hospital.
"We needed to redesign our healthcare services and get acceptance from our physicians. This is the real 'new normal' for us," said Dr Atiporn Ingsathit, deputy director of Ramathibodi Hospital.
More than 5,000 patients, or equivalent to 5% of patients requesting medical services in the last two months, have consulted with the hospital staff through telemedicine. Ramathibodi Hospital plans to increase the shares up to 20% in the near future, said Dr Atiporn.
Telemedicine is organized by having physicians who classify patients base on their health conditions. Patients who have stable conditions are classified as 'Green.' Their appointments with doctors can be delayed, or their cases can be referred to community hospitals near their homes.
Patients with stable conditions but require regular consultants are classified as 'Yellow,' which are the main target for telemedicine service. Patients classified as 'Red' are the ones with unstable conditions. They must visit the hospital even though during the pandemic.
After grouping the patients, physicians pass the information to nurses and the medical record department, of which staff will confirm addresses and phone numbers of patients. Then the hospital staff informs patients about their appointment date via SMS.
Patients can consult physicians via phone calls or VDO call applications. After their consultation sessions end, doctors will upload prescriptions of each case into the hospital's database system.
A finance department will then send medical bills to patients via online platforms, and the latter pay through the e-payment system. Finally, the hospital's pharmacists will ship medicine to patients' addresses the next day.
Dr Jadej Thammathacharee, the NHSO deputy secretary-general, said that Ramathibodi Hospital was a role model for health providers that had been proactive and adaptive to the health crisis.
The hospital also provides health services to beneficiaries of Universal Health Coverage, Thai government's healthcare scheme that guarantees healthcare access to more than 49 million Thais.
The NHSO has encouraged health providers at every level, not just the university hospitals like Ramathibodi Hospital, to launch telemedicine and medicine home delivery services. They can reimburse the cost of service from the NHSO.
"We've supported health providers that are adaptive to the new challenges. Their innovation for health services will improve the quality of healthcare delivery," said Dr Jadej.
VIDEOS
Thailand's UHC Journey
UHC Public relations