Telehealth, telemed, telepharmacy seen as new normal in Universal health Coverage (UHC): NHSO

Telehealth, telemed, telepharmacy seen as new normal in Universal health Coverage (UHC): NHSO
On one hand the Covid-19 outbreak in Thailand had badly disrupted the country’s healthcare system. On the other hand, the public health crisis has been serving as a catalyst for the adoption of modern-day internet-based communication technology as a medium for delivering health and medical care in a long-distance manner.
Three years ago, the National Health Security Office’s (NHSO) interest in new disruption, a hot topic being discussed among many businesses, had driven it to think more seriously as to what could be done more to the country’s healthcare system in order to reap the benefits of the internet technology disruption.

“The businesses were then discussing a lot (about internet technology disruption) and how they were adapting to and benefiting from it. So why didn’t the health care system ride the wave of this development?” said Dr Jadej Thammatacharee, Deputy Secretary-General of the NHSO.
In the beginning, the development of telemedicine in Thailand dealt mainly with case consulting among medical doctors and healthcare staff, without having any patients interact with their doctors through the long-distance system, he said.
Telemedicine is actually not something new in Thailand as it had been experimented around the time the country embraced the satellite technology and the first version of telemedicine back then was conducted through either satellite-based or telephone line connection, he said.
“As mobile phone technology allows better quality of video calls at a far cheaper cost, we saw a greater potential [to develop new telemedicine based on the new mobile phone technology] and began discussing more seriously as to how to implement the idea,” he said.
Old school telemedicine dusted off
In dusting off the old telemedicine project, the main challenge the NHSO aimed to cope with was improve access to and convenience in receiving healthcare services while reducing the number of patients visiting the hospitals under the UHC, he said.
However, the new attempt to develop telemedicine at that time wasn’t making much progress as most of the work dealt mainly with discussions with public and private organisations concerned about the new idea while not really knowing how to effectively implement it at the time, he said.
An enormous challenge then was how to deliver telemedicine without compromising medical standards and medical ethics, he said, adding that enquiries had been made to several professional councils including the Medical Council of Thailand that didn’t really approved the idea at the time.
Covid-19 speeds up telemedicine development
And suddenly the Covid-19 outbreak began hitting the country hard and social distancing was adopted to contain the spread of the new coronavirus that causes the disease as hospitals became places with a high risk of contracting and spreading the virus, he said.
“The situation was unprecedented and came as extraordinary pressure on us. And it therefore drove us back to what we had discussed about previously and brought it back again,” he said. “Telemedicine has overnight become something we have to do and accomplish.”
Dr Jadej described the Covid-19 crisis as an opportunity to push to make telemedicine happen fast and successful in a short period, saying if the Covid-19 outbreak hadn’t erupted, it would have taken at least five years for the country to achieve this level of telemedicine practice.
While the best rate of achievement in telemedicine development in other countries before the Covid-19 pandemic was between 5% and 10% after at least five years of development, the outbreak has forced Thailand to urgently adopt this new form of long-distance medicine, he said.
At the peak of the outbreak, the rate of telemedicine replaced between 40% and 50% of the number out-patient visits by patients with chronic diseases needing regular visits and medication, he said.
A study showed the telemedicine efforts before the Covid-19 pandemic weren’t really successful even in the US, he said.
Ramathibodi moves on to next level
As many large hospitals including Ramathibodi Hospital, Siriraj Hospital and King Chulalongkorn Memorial Hospital have also developed and implemented their own telemedicine systems during the past outbreak, all the NHSO has to do is support them with some funding for services provided to patients under the universal coverage scheme (UCS), he said.
On July 8, 2020 the board of the NHSO approved a proposal to financially support hospitals’ Covid-19 social-distancing in fiscal year 2021 (starting Oct 1, 2020), which applies to not only telemedicine – including home chemotherapy -- for UCS patients but also telehealth that covers a wide range of health promotion activities.
Ramathibodi, for instance, has successfully cut one-thirds of about 4,000 hospital visits by patients with chronic diseases per day at its outpatient ward, he said.

The hospital is now moving on to a second phase of its telemedicine development, which focuses more on so-called “telecare”, said Assoc Prof Atiporn Ingsathit, deputy director of Ramathibodi.
In a medical care programme for patients suspected to have obstructive sleep apnea (OSA), for instance, doctors lend these patients a portable sleep-monitoring device for use at home in a diagnosis of the condition, which normally requires a stay in the hospital, she said.
The provided device is remotely connected to the OSA diagnosis system at the hospital’s sleep apnea clinic via the internet connection, allowing patients’ data collected into the device to be transferred automatically to the clinic and used by its doctors, she said.
And even therapy for OSA can now be performed in a long-distance manner, she said, adding that patients are guided in a video call on how to use a continuous positive airway pressure (CPAP) device properly.
Low investment, high outcome
With the help of high public access to smartphones, the new development of telemedicine doesn’t require much investment on the service provider’s part, while patients can save a great deal of money and time normally spent in travelling to the hospital, said Dr Jadej.
Medicines are delivered to patients seeing their doctors via telemedicine service either by post or through pharmacies taking part in the UHC’s existing medication dispensing programme, he said.
Pursuit of new technology
As part of its primary responsibility to improve public access to healthcare and medical care under the UCS, the NHSO continues working together with its partners in studying all forms of new technology and innovations suitable for adopting under the UHC.
Wearable technology such as medical-grade smartwatches may in the future be given to patients who really need them to closely monitor their vital signs at home to save their lives in an emergency, if proved to be worth investing, he said.
The partners are Health Intervention and Technology Assessment Program (HITAP), Health Systems Research Institute (HSRI), International Health Policy Program (IHPP), said the doctor.
As the Covid-19 pandemic is expected to last at least one to two years from now, he foresaw the internet-based medical and healthcare technology to thrive and be widely adopted in Thailand’s healthcare system.
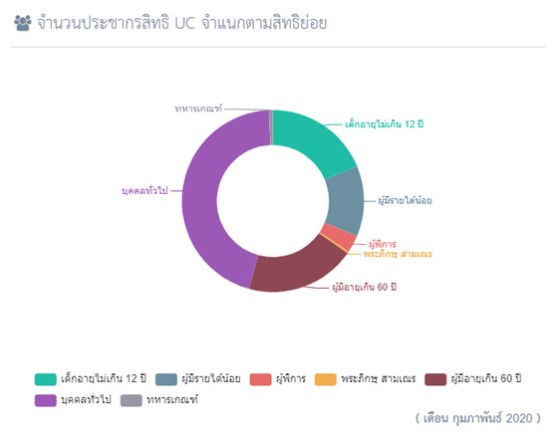
Public Health Minister Anutin Charnvirakul has emphasised with the NHSO that the UC is no longer a healthcare scheme for the poor but a quality one for all, said Dr Jadej.
IN DEPTH
Telehealth, telemed, telepharmacy seen as new normal in Universal health Coverage (UHC): NHSO

Telehealth, telemed, telepharmacy seen as new normal in Universal health Coverage (UHC): NHSO
On one hand the Covid-19 outbreak in Thailand had badly disrupted the country’s healthcare system. On the other hand, the public health crisis has been serving as a catalyst for the adoption of modern-day internet-based communication technology as a medium for delivering health and medical care in a long-distance manner.
Three years ago, the National Health Security Office’s (NHSO) interest in new disruption, a hot topic being discussed among many businesses, had driven it to think more seriously as to what could be done more to the country’s healthcare system in order to reap the benefits of the internet technology disruption.

“The businesses were then discussing a lot (about internet technology disruption) and how they were adapting to and benefiting from it. So why didn’t the health care system ride the wave of this development?” said Dr Jadej Thammatacharee, Deputy Secretary-General of the NHSO.
In the beginning, the development of telemedicine in Thailand dealt mainly with case consulting among medical doctors and healthcare staff, without having any patients interact with their doctors through the long-distance system, he said.
Telemedicine is actually not something new in Thailand as it had been experimented around the time the country embraced the satellite technology and the first version of telemedicine back then was conducted through either satellite-based or telephone line connection, he said.
“As mobile phone technology allows better quality of video calls at a far cheaper cost, we saw a greater potential [to develop new telemedicine based on the new mobile phone technology] and began discussing more seriously as to how to implement the idea,” he said.
Old school telemedicine dusted off
In dusting off the old telemedicine project, the main challenge the NHSO aimed to cope with was improve access to and convenience in receiving healthcare services while reducing the number of patients visiting the hospitals under the UHC, he said.
However, the new attempt to develop telemedicine at that time wasn’t making much progress as most of the work dealt mainly with discussions with public and private organisations concerned about the new idea while not really knowing how to effectively implement it at the time, he said.
An enormous challenge then was how to deliver telemedicine without compromising medical standards and medical ethics, he said, adding that enquiries had been made to several professional councils including the Medical Council of Thailand that didn’t really approved the idea at the time.
Covid-19 speeds up telemedicine development
And suddenly the Covid-19 outbreak began hitting the country hard and social distancing was adopted to contain the spread of the new coronavirus that causes the disease as hospitals became places with a high risk of contracting and spreading the virus, he said.
“The situation was unprecedented and came as extraordinary pressure on us. And it therefore drove us back to what we had discussed about previously and brought it back again,” he said. “Telemedicine has overnight become something we have to do and accomplish.”
Dr Jadej described the Covid-19 crisis as an opportunity to push to make telemedicine happen fast and successful in a short period, saying if the Covid-19 outbreak hadn’t erupted, it would have taken at least five years for the country to achieve this level of telemedicine practice.
While the best rate of achievement in telemedicine development in other countries before the Covid-19 pandemic was between 5% and 10% after at least five years of development, the outbreak has forced Thailand to urgently adopt this new form of long-distance medicine, he said.
At the peak of the outbreak, the rate of telemedicine replaced between 40% and 50% of the number out-patient visits by patients with chronic diseases needing regular visits and medication, he said.
A study showed the telemedicine efforts before the Covid-19 pandemic weren’t really successful even in the US, he said.
Ramathibodi moves on to next level
As many large hospitals including Ramathibodi Hospital, Siriraj Hospital and King Chulalongkorn Memorial Hospital have also developed and implemented their own telemedicine systems during the past outbreak, all the NHSO has to do is support them with some funding for services provided to patients under the universal coverage scheme (UCS), he said.
On July 8, 2020 the board of the NHSO approved a proposal to financially support hospitals’ Covid-19 social-distancing in fiscal year 2021 (starting Oct 1, 2020), which applies to not only telemedicine – including home chemotherapy -- for UCS patients but also telehealth that covers a wide range of health promotion activities.
Ramathibodi, for instance, has successfully cut one-thirds of about 4,000 hospital visits by patients with chronic diseases per day at its outpatient ward, he said.

The hospital is now moving on to a second phase of its telemedicine development, which focuses more on so-called “telecare”, said Assoc Prof Atiporn Ingsathit, deputy director of Ramathibodi.
In a medical care programme for patients suspected to have obstructive sleep apnea (OSA), for instance, doctors lend these patients a portable sleep-monitoring device for use at home in a diagnosis of the condition, which normally requires a stay in the hospital, she said.
The provided device is remotely connected to the OSA diagnosis system at the hospital’s sleep apnea clinic via the internet connection, allowing patients’ data collected into the device to be transferred automatically to the clinic and used by its doctors, she said.
And even therapy for OSA can now be performed in a long-distance manner, she said, adding that patients are guided in a video call on how to use a continuous positive airway pressure (CPAP) device properly.
Low investment, high outcome
With the help of high public access to smartphones, the new development of telemedicine doesn’t require much investment on the service provider’s part, while patients can save a great deal of money and time normally spent in travelling to the hospital, said Dr Jadej.
Medicines are delivered to patients seeing their doctors via telemedicine service either by post or through pharmacies taking part in the UHC’s existing medication dispensing programme, he said.
Pursuit of new technology
As part of its primary responsibility to improve public access to healthcare and medical care under the UCS, the NHSO continues working together with its partners in studying all forms of new technology and innovations suitable for adopting under the UHC.
Wearable technology such as medical-grade smartwatches may in the future be given to patients who really need them to closely monitor their vital signs at home to save their lives in an emergency, if proved to be worth investing, he said.
The partners are Health Intervention and Technology Assessment Program (HITAP), Health Systems Research Institute (HSRI), International Health Policy Program (IHPP), said the doctor.
As the Covid-19 pandemic is expected to last at least one to two years from now, he foresaw the internet-based medical and healthcare technology to thrive and be widely adopted in Thailand’s healthcare system.
Public Health Minister Anutin Charnvirakul has emphasised with the NHSO that the UC is no longer a healthcare scheme for the poor but a quality one for all, said Dr Jadej.
Events
Telehealth, telemed, telepharmacy seen as new normal in Universal health Coverage (UHC): NHSO

Telehealth, telemed, telepharmacy seen as new normal in Universal health Coverage (UHC): NHSO
On one hand the Covid-19 outbreak in Thailand had badly disrupted the country’s healthcare system. On the other hand, the public health crisis has been serving as a catalyst for the adoption of modern-day internet-based communication technology as a medium for delivering health and medical care in a long-distance manner.
Three years ago, the National Health Security Office’s (NHSO) interest in new disruption, a hot topic being discussed among many businesses, had driven it to think more seriously as to what could be done more to the country’s healthcare system in order to reap the benefits of the internet technology disruption.

“The businesses were then discussing a lot (about internet technology disruption) and how they were adapting to and benefiting from it. So why didn’t the health care system ride the wave of this development?” said Dr Jadej Thammatacharee, Deputy Secretary-General of the NHSO.
In the beginning, the development of telemedicine in Thailand dealt mainly with case consulting among medical doctors and healthcare staff, without having any patients interact with their doctors through the long-distance system, he said.
Telemedicine is actually not something new in Thailand as it had been experimented around the time the country embraced the satellite technology and the first version of telemedicine back then was conducted through either satellite-based or telephone line connection, he said.
“As mobile phone technology allows better quality of video calls at a far cheaper cost, we saw a greater potential [to develop new telemedicine based on the new mobile phone technology] and began discussing more seriously as to how to implement the idea,” he said.
Old school telemedicine dusted off
In dusting off the old telemedicine project, the main challenge the NHSO aimed to cope with was improve access to and convenience in receiving healthcare services while reducing the number of patients visiting the hospitals under the UHC, he said.
However, the new attempt to develop telemedicine at that time wasn’t making much progress as most of the work dealt mainly with discussions with public and private organisations concerned about the new idea while not really knowing how to effectively implement it at the time, he said.
An enormous challenge then was how to deliver telemedicine without compromising medical standards and medical ethics, he said, adding that enquiries had been made to several professional councils including the Medical Council of Thailand that didn’t really approved the idea at the time.
Covid-19 speeds up telemedicine development
And suddenly the Covid-19 outbreak began hitting the country hard and social distancing was adopted to contain the spread of the new coronavirus that causes the disease as hospitals became places with a high risk of contracting and spreading the virus, he said.
“The situation was unprecedented and came as extraordinary pressure on us. And it therefore drove us back to what we had discussed about previously and brought it back again,” he said. “Telemedicine has overnight become something we have to do and accomplish.”
Dr Jadej described the Covid-19 crisis as an opportunity to push to make telemedicine happen fast and successful in a short period, saying if the Covid-19 outbreak hadn’t erupted, it would have taken at least five years for the country to achieve this level of telemedicine practice.
While the best rate of achievement in telemedicine development in other countries before the Covid-19 pandemic was between 5% and 10% after at least five years of development, the outbreak has forced Thailand to urgently adopt this new form of long-distance medicine, he said.
At the peak of the outbreak, the rate of telemedicine replaced between 40% and 50% of the number out-patient visits by patients with chronic diseases needing regular visits and medication, he said.
A study showed the telemedicine efforts before the Covid-19 pandemic weren’t really successful even in the US, he said.
Ramathibodi moves on to next level
As many large hospitals including Ramathibodi Hospital, Siriraj Hospital and King Chulalongkorn Memorial Hospital have also developed and implemented their own telemedicine systems during the past outbreak, all the NHSO has to do is support them with some funding for services provided to patients under the universal coverage scheme (UCS), he said.
On July 8, 2020 the board of the NHSO approved a proposal to financially support hospitals’ Covid-19 social-distancing in fiscal year 2021 (starting Oct 1, 2020), which applies to not only telemedicine – including home chemotherapy -- for UCS patients but also telehealth that covers a wide range of health promotion activities.
Ramathibodi, for instance, has successfully cut one-thirds of about 4,000 hospital visits by patients with chronic diseases per day at its outpatient ward, he said.

The hospital is now moving on to a second phase of its telemedicine development, which focuses more on so-called “telecare”, said Assoc Prof Atiporn Ingsathit, deputy director of Ramathibodi.
In a medical care programme for patients suspected to have obstructive sleep apnea (OSA), for instance, doctors lend these patients a portable sleep-monitoring device for use at home in a diagnosis of the condition, which normally requires a stay in the hospital, she said.
The provided device is remotely connected to the OSA diagnosis system at the hospital’s sleep apnea clinic via the internet connection, allowing patients’ data collected into the device to be transferred automatically to the clinic and used by its doctors, she said.
And even therapy for OSA can now be performed in a long-distance manner, she said, adding that patients are guided in a video call on how to use a continuous positive airway pressure (CPAP) device properly.
Low investment, high outcome
With the help of high public access to smartphones, the new development of telemedicine doesn’t require much investment on the service provider’s part, while patients can save a great deal of money and time normally spent in travelling to the hospital, said Dr Jadej.
Medicines are delivered to patients seeing their doctors via telemedicine service either by post or through pharmacies taking part in the UHC’s existing medication dispensing programme, he said.
Pursuit of new technology
As part of its primary responsibility to improve public access to healthcare and medical care under the UCS, the NHSO continues working together with its partners in studying all forms of new technology and innovations suitable for adopting under the UHC.
Wearable technology such as medical-grade smartwatches may in the future be given to patients who really need them to closely monitor their vital signs at home to save their lives in an emergency, if proved to be worth investing, he said.
The partners are Health Intervention and Technology Assessment Program (HITAP), Health Systems Research Institute (HSRI), International Health Policy Program (IHPP), said the doctor.
As the Covid-19 pandemic is expected to last at least one to two years from now, he foresaw the internet-based medical and healthcare technology to thrive and be widely adopted in Thailand’s healthcare system.
Public Health Minister Anutin Charnvirakul has emphasised with the NHSO that the UC is no longer a healthcare scheme for the poor but a quality one for all, said Dr Jadej.
RESOURCE CENTER
SECRETARY-GENERAL
Telehealth, telemed, telepharmacy seen as new normal in Universal health Coverage (UHC): NHSO

Telehealth, telemed, telepharmacy seen as new normal in Universal health Coverage (UHC): NHSO
On one hand the Covid-19 outbreak in Thailand had badly disrupted the country’s healthcare system. On the other hand, the public health crisis has been serving as a catalyst for the adoption of modern-day internet-based communication technology as a medium for delivering health and medical care in a long-distance manner.
Three years ago, the National Health Security Office’s (NHSO) interest in new disruption, a hot topic being discussed among many businesses, had driven it to think more seriously as to what could be done more to the country’s healthcare system in order to reap the benefits of the internet technology disruption.

“The businesses were then discussing a lot (about internet technology disruption) and how they were adapting to and benefiting from it. So why didn’t the health care system ride the wave of this development?” said Dr Jadej Thammatacharee, Deputy Secretary-General of the NHSO.
In the beginning, the development of telemedicine in Thailand dealt mainly with case consulting among medical doctors and healthcare staff, without having any patients interact with their doctors through the long-distance system, he said.
Telemedicine is actually not something new in Thailand as it had been experimented around the time the country embraced the satellite technology and the first version of telemedicine back then was conducted through either satellite-based or telephone line connection, he said.
“As mobile phone technology allows better quality of video calls at a far cheaper cost, we saw a greater potential [to develop new telemedicine based on the new mobile phone technology] and began discussing more seriously as to how to implement the idea,” he said.
Old school telemedicine dusted off
In dusting off the old telemedicine project, the main challenge the NHSO aimed to cope with was improve access to and convenience in receiving healthcare services while reducing the number of patients visiting the hospitals under the UHC, he said.
However, the new attempt to develop telemedicine at that time wasn’t making much progress as most of the work dealt mainly with discussions with public and private organisations concerned about the new idea while not really knowing how to effectively implement it at the time, he said.
An enormous challenge then was how to deliver telemedicine without compromising medical standards and medical ethics, he said, adding that enquiries had been made to several professional councils including the Medical Council of Thailand that didn’t really approved the idea at the time.
Covid-19 speeds up telemedicine development
And suddenly the Covid-19 outbreak began hitting the country hard and social distancing was adopted to contain the spread of the new coronavirus that causes the disease as hospitals became places with a high risk of contracting and spreading the virus, he said.
“The situation was unprecedented and came as extraordinary pressure on us. And it therefore drove us back to what we had discussed about previously and brought it back again,” he said. “Telemedicine has overnight become something we have to do and accomplish.”
Dr Jadej described the Covid-19 crisis as an opportunity to push to make telemedicine happen fast and successful in a short period, saying if the Covid-19 outbreak hadn’t erupted, it would have taken at least five years for the country to achieve this level of telemedicine practice.
While the best rate of achievement in telemedicine development in other countries before the Covid-19 pandemic was between 5% and 10% after at least five years of development, the outbreak has forced Thailand to urgently adopt this new form of long-distance medicine, he said.
At the peak of the outbreak, the rate of telemedicine replaced between 40% and 50% of the number out-patient visits by patients with chronic diseases needing regular visits and medication, he said.
A study showed the telemedicine efforts before the Covid-19 pandemic weren’t really successful even in the US, he said.
Ramathibodi moves on to next level
As many large hospitals including Ramathibodi Hospital, Siriraj Hospital and King Chulalongkorn Memorial Hospital have also developed and implemented their own telemedicine systems during the past outbreak, all the NHSO has to do is support them with some funding for services provided to patients under the universal coverage scheme (UCS), he said.
On July 8, 2020 the board of the NHSO approved a proposal to financially support hospitals’ Covid-19 social-distancing in fiscal year 2021 (starting Oct 1, 2020), which applies to not only telemedicine – including home chemotherapy -- for UCS patients but also telehealth that covers a wide range of health promotion activities.
Ramathibodi, for instance, has successfully cut one-thirds of about 4,000 hospital visits by patients with chronic diseases per day at its outpatient ward, he said.

The hospital is now moving on to a second phase of its telemedicine development, which focuses more on so-called “telecare”, said Assoc Prof Atiporn Ingsathit, deputy director of Ramathibodi.
In a medical care programme for patients suspected to have obstructive sleep apnea (OSA), for instance, doctors lend these patients a portable sleep-monitoring device for use at home in a diagnosis of the condition, which normally requires a stay in the hospital, she said.
The provided device is remotely connected to the OSA diagnosis system at the hospital’s sleep apnea clinic via the internet connection, allowing patients’ data collected into the device to be transferred automatically to the clinic and used by its doctors, she said.
And even therapy for OSA can now be performed in a long-distance manner, she said, adding that patients are guided in a video call on how to use a continuous positive airway pressure (CPAP) device properly.
Low investment, high outcome
With the help of high public access to smartphones, the new development of telemedicine doesn’t require much investment on the service provider’s part, while patients can save a great deal of money and time normally spent in travelling to the hospital, said Dr Jadej.
Medicines are delivered to patients seeing their doctors via telemedicine service either by post or through pharmacies taking part in the UHC’s existing medication dispensing programme, he said.
Pursuit of new technology
As part of its primary responsibility to improve public access to healthcare and medical care under the UCS, the NHSO continues working together with its partners in studying all forms of new technology and innovations suitable for adopting under the UHC.
Wearable technology such as medical-grade smartwatches may in the future be given to patients who really need them to closely monitor their vital signs at home to save their lives in an emergency, if proved to be worth investing, he said.
The partners are Health Intervention and Technology Assessment Program (HITAP), Health Systems Research Institute (HSRI), International Health Policy Program (IHPP), said the doctor.
As the Covid-19 pandemic is expected to last at least one to two years from now, he foresaw the internet-based medical and healthcare technology to thrive and be widely adopted in Thailand’s healthcare system.
Public Health Minister Anutin Charnvirakul has emphasised with the NHSO that the UC is no longer a healthcare scheme for the poor but a quality one for all, said Dr Jadej.
VIDEOS
Thailand's UHC Journey
UHC Public relations