Thailand to share knowhow of DRG payment system
.jpg) An exclusive interview with NHSO deputy secretary-general Dr. Jadej Thammatacharee
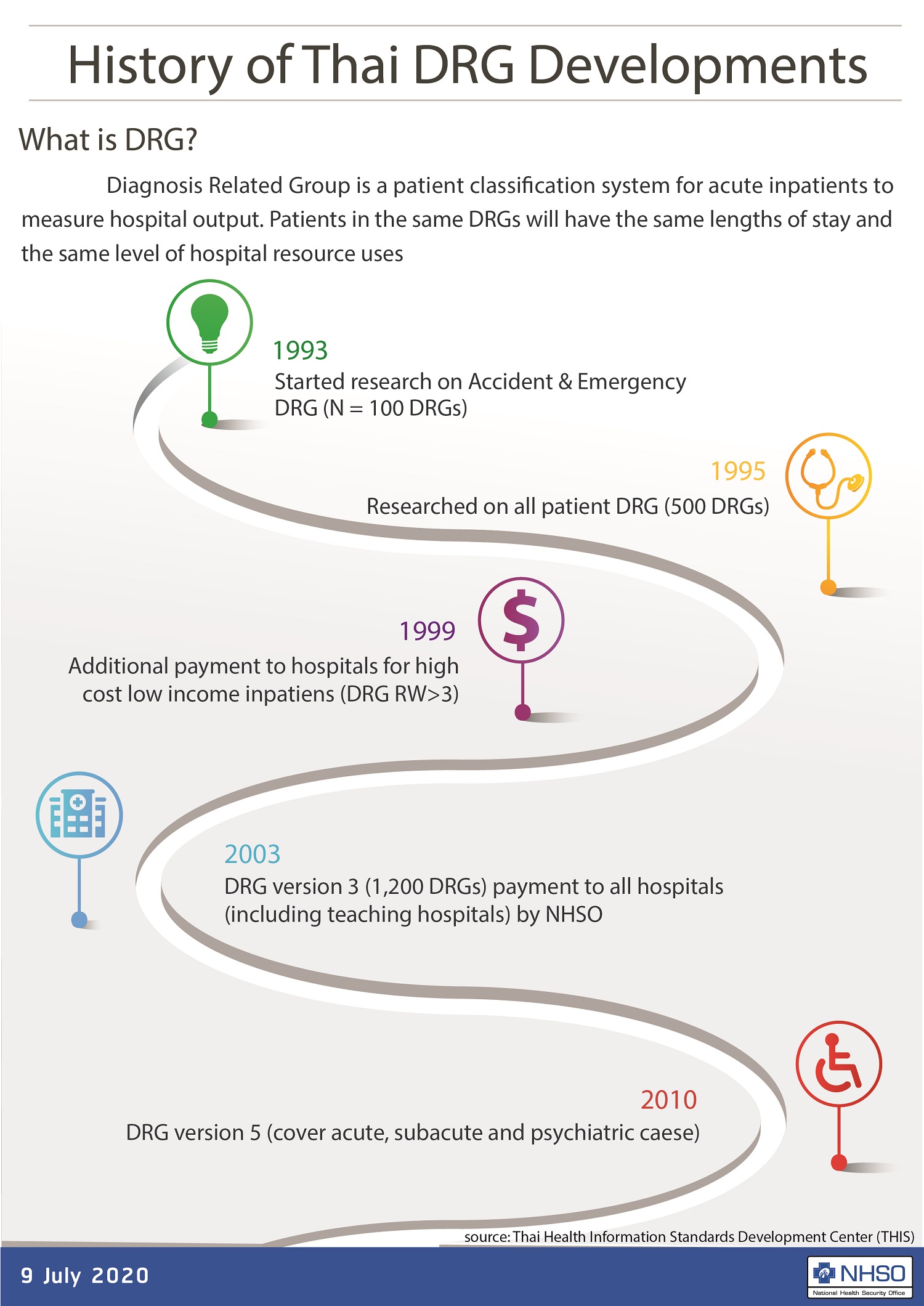
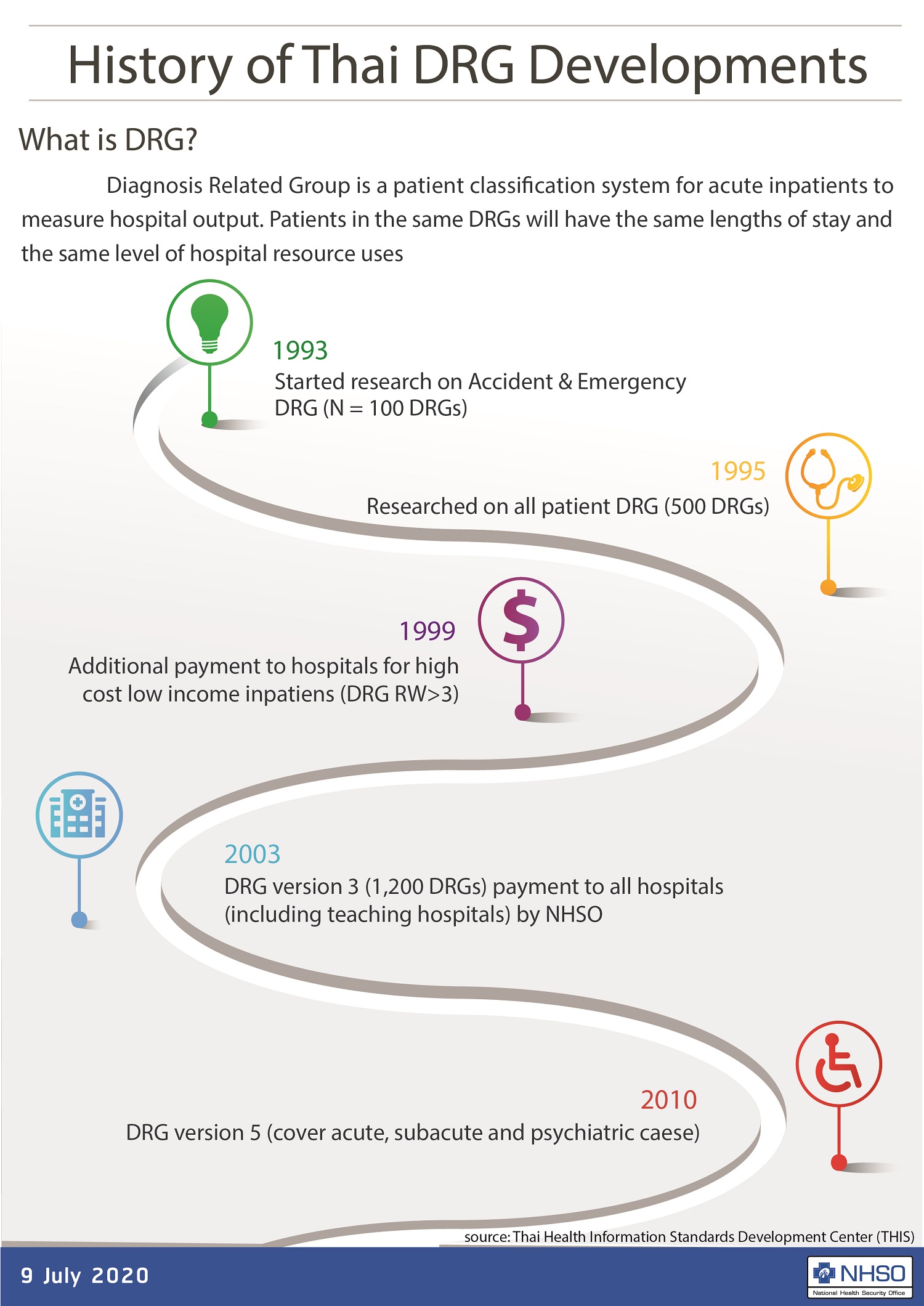
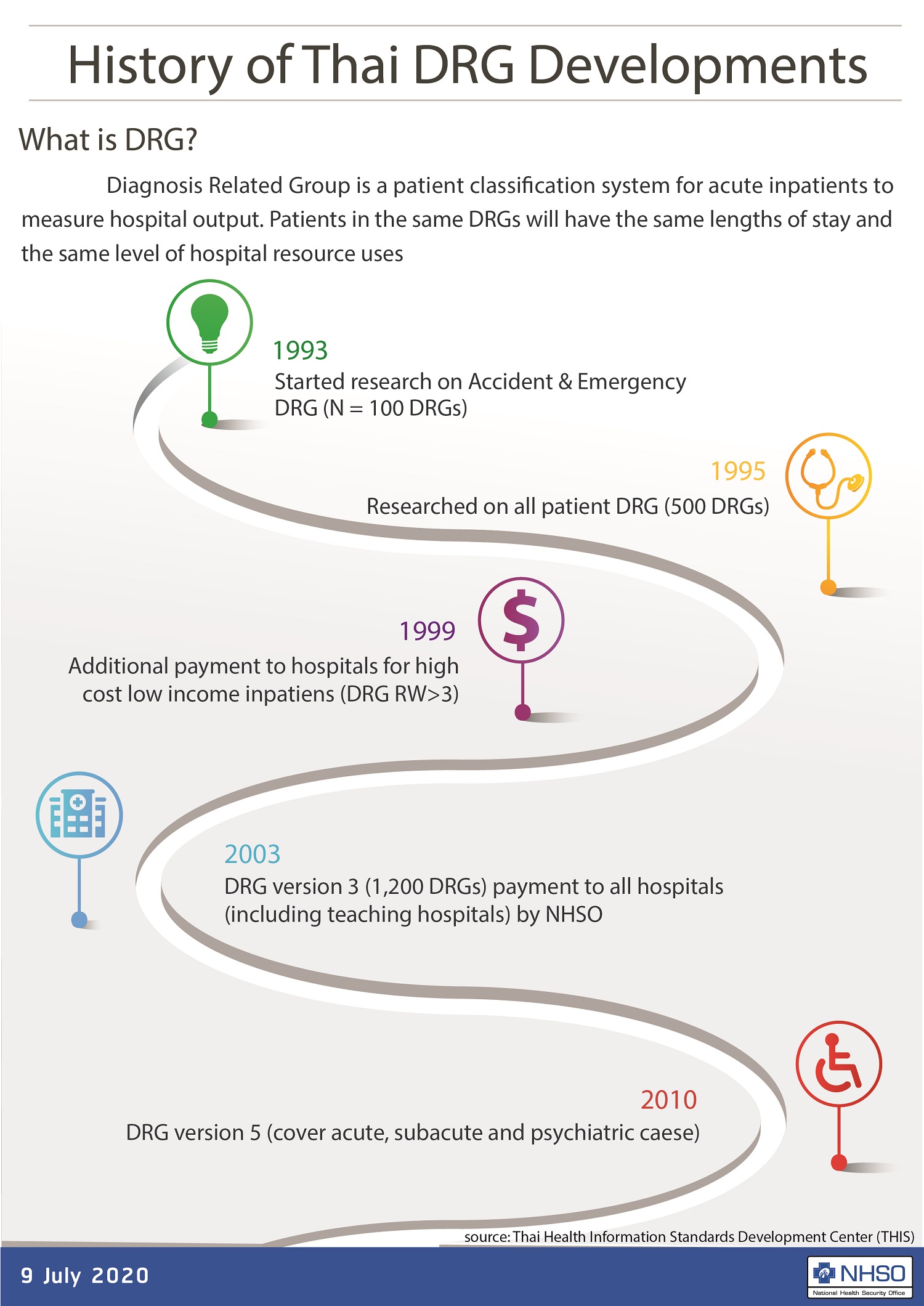
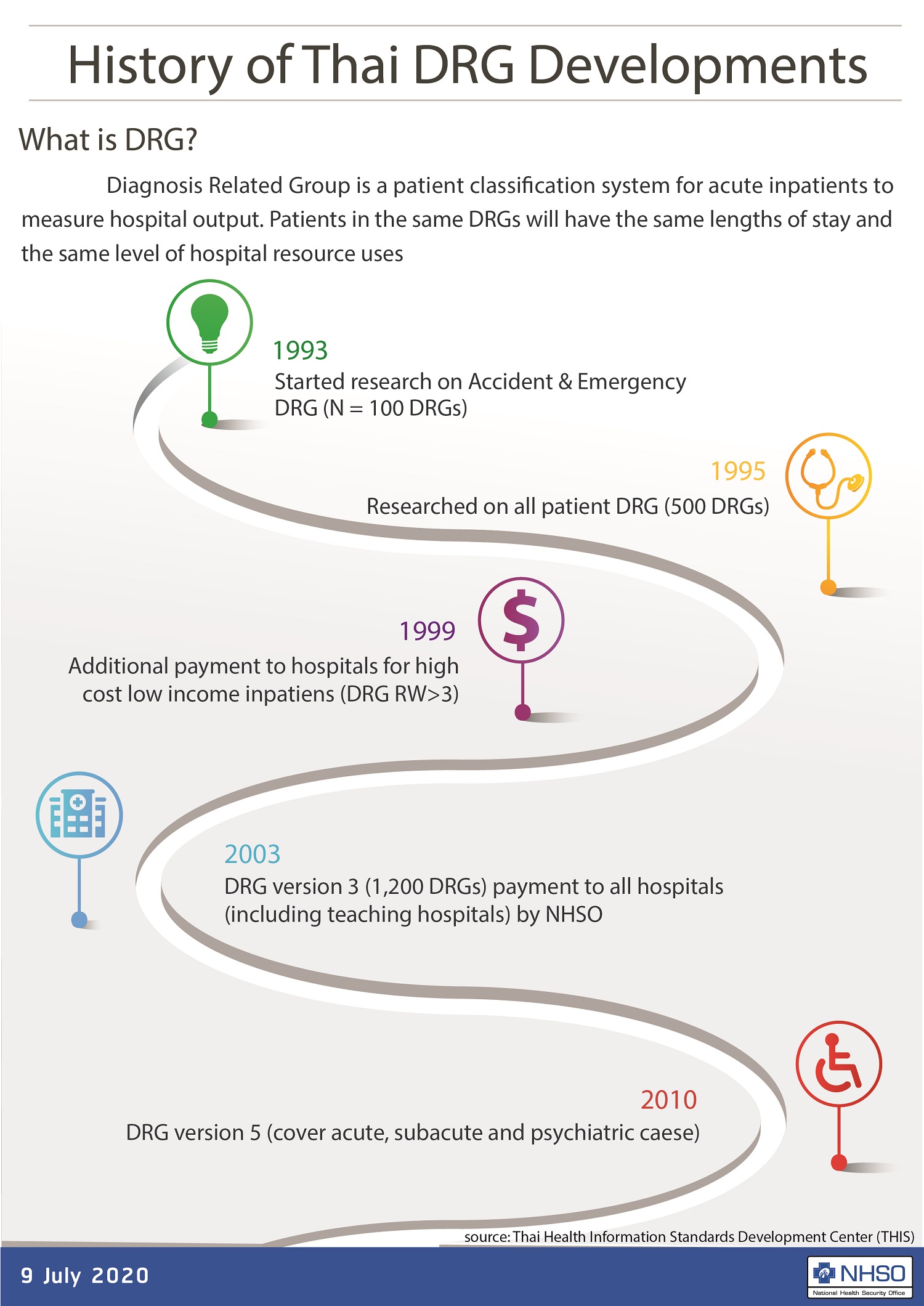
An exclusive interview with NHSO deputy secretary-general Dr. Jadej ThammatachareeDiagnosis-related group (DRG) is an essential payment method for universal healthcare coverage that enhances efficiency and sustainability of health spending, as well as overcome escalating healthcare costs.
In 2003, Thai National Health Security Office (NHSO) introduced DRG in the Universal Coverage Scheme (UCS) 's reimbursement system. The adoption of DRG was later extended to other two Thai health benefit schemes---Social Security Scheme and Civil Servant Medical Benefit Scheme.
Dr. Jadej Thammatacharee, NHSO deputy secretary-general, explains the development of DRG in the Thai healthcare system, and the NHSO's intention to share know-how with any developing countries that plan to establish universal healthcare coverage.
What is DRG?
Dr. Jadej: DRG is inpatient prospective payment system that categorizes hospitalization costs and determines how much to pay.
Traditionally, physicians and health providers charge patients on a case-by-case basis. Consequently, medical fees are not standardizing, and they can be varied in each patient case.
This challenge led to the invention of DRG, firstly introduced in the United States in 1983, to create a "fair" payment system in which patients and the governments (that run health insurance programs) can identify the sources of medical fees and pay reasonable prices.
How does DRG function in healthcare system?
Dr. Jadej: Let's think about eggs. Hens lay eggs in various sizes. To sell eggs, merchants must group eggs in similar sizes, then assign numbers to them. A group of the largest-sized eggs gets number 1. The smaller ones get number 2, 3, and so on.
We can compare the classification of egg sizes with the principle of DRG. There are more than 40,000 diseases in this world. If health providers charge patients base on the care of each illness, the medical bills of each patient will load with lists of numerous items.
To pay hospitals under this circumstance, the government staff must work on identifying the items in each medical bill, which is very time-consuming and costly.
This problem is solved by DRG payment system. Like grouping eggs by their sizes, the diseases are grouped base on the average resources required to care for those diseases.
For example, appendectomy and colonoscopy are arranged in the same category because health providers use similar resources to provide the services. For Thailand, a myriad of diseases are categorized into 2,500 groups.
Then DRG weight is assigned for each disease group. The higher the DRG weight, the more resources are required to treat a patient, meaning the more expensive medical fees. Medical cost is determined by multiplying DRG weight by cost per relative weight of disease.
Why is DRG payment system essential to the Thai healthcare system?
Dr. Jadej: DRG is applied in inpatient care reimbursement, to replace cost-based reimbursement that had been used widely in the past.
Before the introduction of DRG, Thai healthcare reimbursement was based on fee-for-service system---a traditional payment model where services healthcare providers are reimbursed on the basis of the number of services they provide.
Fee-for-service system undermines the Thai healthcare system by hiking the cost of health service and administrative works. It also encourages physicians to deliver unnecessary care to maximize their profit.
On the other hands, DRG payment system can control healthcare expenses more efficiently, and make sure that Thai healthcare schemes will not go bankrupt by unnecessary medical costs.
How could Thailand succeed in developing DRG model?
Dr. Jadej: During a period of Thai healthcare reform more than two decades ago, we thought about adopting DRG model from the United States. But we needed to buy the model license from an American company, which was unaffordable for us at the time.
Fortunately, Thailand had many talented health researchers. A group of researchers led by Dr. Supasit Pannarunothai took an initiate in developing and modifying Thai-version DRG since the early 1990s, with supports from Health Systems Research Institute and the NHSO.
The UCS, cover health benefit for 49 million Thais, was the first of the Thai health benefit schemes to adopt DRG for inpatient services in 2003. The government's other two healthcare schemes, Social Security Scheme and Civil Servant Medical Benefit Scheme followed in the late 2000s.
The process of DRG development needs participation from health providers. Therefore, we must hold discussions with hospital representatives each year to get their feedback and update the disease classification.
What is the latest progress of Thai DRG?
Dr. Jadej: We have received some good feedback from international organizations, including the World Bank Group that encourages Thailand to take the lead in DRG development for ASEAN countries.
Recently, the Philippines and Vietnam have approached us and shown their interest in using Thai-version DRG. They are at the beginning stage of introducing universal healthcare coverage to their populations, so they need to reform their health financing.
We're aware that DRG is a financial method necessary for starting universal healthcare coverage in developing countries. We are willing to share our resources and our Thai-version DRG without charging any intellectual property fees. We want to be a part of the global effort to achieve universal healthcare coverage in the coming years.
IN DEPTH
Thailand to share knowhow of DRG payment system
.jpg) An exclusive interview with NHSO deputy secretary-general Dr. Jadej Thammatacharee
An exclusive interview with NHSO deputy secretary-general Dr. Jadej ThammatachareeDiagnosis-related group (DRG) is an essential payment method for universal healthcare coverage that enhances efficiency and sustainability of health spending, as well as overcome escalating healthcare costs.
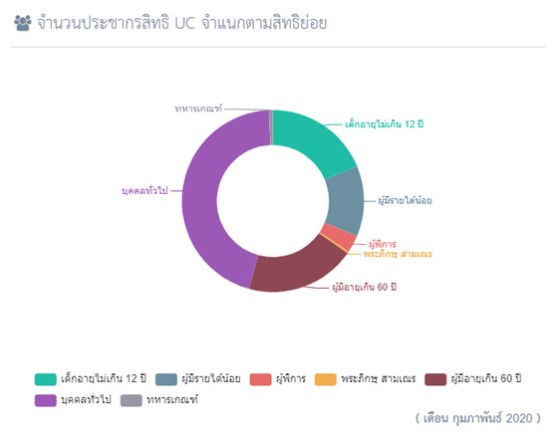
In 2003, Thai National Health Security Office (NHSO) introduced DRG in the Universal Coverage Scheme (UCS) 's reimbursement system. The adoption of DRG was later extended to other two Thai health benefit schemes---Social Security Scheme and Civil Servant Medical Benefit Scheme.
Dr. Jadej Thammatacharee, NHSO deputy secretary-general, explains the development of DRG in the Thai healthcare system, and the NHSO's intention to share know-how with any developing countries that plan to establish universal healthcare coverage.
What is DRG?
Dr. Jadej: DRG is inpatient prospective payment system that categorizes hospitalization costs and determines how much to pay.
Traditionally, physicians and health providers charge patients on a case-by-case basis. Consequently, medical fees are not standardizing, and they can be varied in each patient case.
This challenge led to the invention of DRG, firstly introduced in the United States in 1983, to create a "fair" payment system in which patients and the governments (that run health insurance programs) can identify the sources of medical fees and pay reasonable prices.
How does DRG function in healthcare system?
Dr. Jadej: Let's think about eggs. Hens lay eggs in various sizes. To sell eggs, merchants must group eggs in similar sizes, then assign numbers to them. A group of the largest-sized eggs gets number 1. The smaller ones get number 2, 3, and so on.
We can compare the classification of egg sizes with the principle of DRG. There are more than 40,000 diseases in this world. If health providers charge patients base on the care of each illness, the medical bills of each patient will load with lists of numerous items.
To pay hospitals under this circumstance, the government staff must work on identifying the items in each medical bill, which is very time-consuming and costly.
This problem is solved by DRG payment system. Like grouping eggs by their sizes, the diseases are grouped base on the average resources required to care for those diseases.
For example, appendectomy and colonoscopy are arranged in the same category because health providers use similar resources to provide the services. For Thailand, a myriad of diseases are categorized into 2,500 groups.
Then DRG weight is assigned for each disease group. The higher the DRG weight, the more resources are required to treat a patient, meaning the more expensive medical fees. Medical cost is determined by multiplying DRG weight by cost per relative weight of disease.
Why is DRG payment system essential to the Thai healthcare system?
Dr. Jadej: DRG is applied in inpatient care reimbursement, to replace cost-based reimbursement that had been used widely in the past.
Before the introduction of DRG, Thai healthcare reimbursement was based on fee-for-service system---a traditional payment model where services healthcare providers are reimbursed on the basis of the number of services they provide.
Fee-for-service system undermines the Thai healthcare system by hiking the cost of health service and administrative works. It also encourages physicians to deliver unnecessary care to maximize their profit.
On the other hands, DRG payment system can control healthcare expenses more efficiently, and make sure that Thai healthcare schemes will not go bankrupt by unnecessary medical costs.
How could Thailand succeed in developing DRG model?
Dr. Jadej: During a period of Thai healthcare reform more than two decades ago, we thought about adopting DRG model from the United States. But we needed to buy the model license from an American company, which was unaffordable for us at the time.
Fortunately, Thailand had many talented health researchers. A group of researchers led by Dr. Supasit Pannarunothai took an initiate in developing and modifying Thai-version DRG since the early 1990s, with supports from Health Systems Research Institute and the NHSO.
The UCS, cover health benefit for 49 million Thais, was the first of the Thai health benefit schemes to adopt DRG for inpatient services in 2003. The government's other two healthcare schemes, Social Security Scheme and Civil Servant Medical Benefit Scheme followed in the late 2000s.
The process of DRG development needs participation from health providers. Therefore, we must hold discussions with hospital representatives each year to get their feedback and update the disease classification.
What is the latest progress of Thai DRG?
Dr. Jadej: We have received some good feedback from international organizations, including the World Bank Group that encourages Thailand to take the lead in DRG development for ASEAN countries.
Recently, the Philippines and Vietnam have approached us and shown their interest in using Thai-version DRG. They are at the beginning stage of introducing universal healthcare coverage to their populations, so they need to reform their health financing.
We're aware that DRG is a financial method necessary for starting universal healthcare coverage in developing countries. We are willing to share our resources and our Thai-version DRG without charging any intellectual property fees. We want to be a part of the global effort to achieve universal healthcare coverage in the coming years.
Events
Thailand to share knowhow of DRG payment system
.jpg) An exclusive interview with NHSO deputy secretary-general Dr. Jadej Thammatacharee
An exclusive interview with NHSO deputy secretary-general Dr. Jadej ThammatachareeDiagnosis-related group (DRG) is an essential payment method for universal healthcare coverage that enhances efficiency and sustainability of health spending, as well as overcome escalating healthcare costs.
In 2003, Thai National Health Security Office (NHSO) introduced DRG in the Universal Coverage Scheme (UCS) 's reimbursement system. The adoption of DRG was later extended to other two Thai health benefit schemes---Social Security Scheme and Civil Servant Medical Benefit Scheme.
Dr. Jadej Thammatacharee, NHSO deputy secretary-general, explains the development of DRG in the Thai healthcare system, and the NHSO's intention to share know-how with any developing countries that plan to establish universal healthcare coverage.
What is DRG?
Dr. Jadej: DRG is inpatient prospective payment system that categorizes hospitalization costs and determines how much to pay.
Traditionally, physicians and health providers charge patients on a case-by-case basis. Consequently, medical fees are not standardizing, and they can be varied in each patient case.
This challenge led to the invention of DRG, firstly introduced in the United States in 1983, to create a "fair" payment system in which patients and the governments (that run health insurance programs) can identify the sources of medical fees and pay reasonable prices.
How does DRG function in healthcare system?
Dr. Jadej: Let's think about eggs. Hens lay eggs in various sizes. To sell eggs, merchants must group eggs in similar sizes, then assign numbers to them. A group of the largest-sized eggs gets number 1. The smaller ones get number 2, 3, and so on.
We can compare the classification of egg sizes with the principle of DRG. There are more than 40,000 diseases in this world. If health providers charge patients base on the care of each illness, the medical bills of each patient will load with lists of numerous items.
To pay hospitals under this circumstance, the government staff must work on identifying the items in each medical bill, which is very time-consuming and costly.
This problem is solved by DRG payment system. Like grouping eggs by their sizes, the diseases are grouped base on the average resources required to care for those diseases.
For example, appendectomy and colonoscopy are arranged in the same category because health providers use similar resources to provide the services. For Thailand, a myriad of diseases are categorized into 2,500 groups.
Then DRG weight is assigned for each disease group. The higher the DRG weight, the more resources are required to treat a patient, meaning the more expensive medical fees. Medical cost is determined by multiplying DRG weight by cost per relative weight of disease.
Why is DRG payment system essential to the Thai healthcare system?
Dr. Jadej: DRG is applied in inpatient care reimbursement, to replace cost-based reimbursement that had been used widely in the past.
Before the introduction of DRG, Thai healthcare reimbursement was based on fee-for-service system---a traditional payment model where services healthcare providers are reimbursed on the basis of the number of services they provide.
Fee-for-service system undermines the Thai healthcare system by hiking the cost of health service and administrative works. It also encourages physicians to deliver unnecessary care to maximize their profit.
On the other hands, DRG payment system can control healthcare expenses more efficiently, and make sure that Thai healthcare schemes will not go bankrupt by unnecessary medical costs.
How could Thailand succeed in developing DRG model?
Dr. Jadej: During a period of Thai healthcare reform more than two decades ago, we thought about adopting DRG model from the United States. But we needed to buy the model license from an American company, which was unaffordable for us at the time.
Fortunately, Thailand had many talented health researchers. A group of researchers led by Dr. Supasit Pannarunothai took an initiate in developing and modifying Thai-version DRG since the early 1990s, with supports from Health Systems Research Institute and the NHSO.
The UCS, cover health benefit for 49 million Thais, was the first of the Thai health benefit schemes to adopt DRG for inpatient services in 2003. The government's other two healthcare schemes, Social Security Scheme and Civil Servant Medical Benefit Scheme followed in the late 2000s.
The process of DRG development needs participation from health providers. Therefore, we must hold discussions with hospital representatives each year to get their feedback and update the disease classification.
What is the latest progress of Thai DRG?
Dr. Jadej: We have received some good feedback from international organizations, including the World Bank Group that encourages Thailand to take the lead in DRG development for ASEAN countries.
Recently, the Philippines and Vietnam have approached us and shown their interest in using Thai-version DRG. They are at the beginning stage of introducing universal healthcare coverage to their populations, so they need to reform their health financing.
We're aware that DRG is a financial method necessary for starting universal healthcare coverage in developing countries. We are willing to share our resources and our Thai-version DRG without charging any intellectual property fees. We want to be a part of the global effort to achieve universal healthcare coverage in the coming years.
RESOURCE CENTER
SECRETARY-GENERAL
Thailand to share knowhow of DRG payment system
.jpg) An exclusive interview with NHSO deputy secretary-general Dr. Jadej Thammatacharee
An exclusive interview with NHSO deputy secretary-general Dr. Jadej ThammatachareeDiagnosis-related group (DRG) is an essential payment method for universal healthcare coverage that enhances efficiency and sustainability of health spending, as well as overcome escalating healthcare costs.
In 2003, Thai National Health Security Office (NHSO) introduced DRG in the Universal Coverage Scheme (UCS) 's reimbursement system. The adoption of DRG was later extended to other two Thai health benefit schemes---Social Security Scheme and Civil Servant Medical Benefit Scheme.
Dr. Jadej Thammatacharee, NHSO deputy secretary-general, explains the development of DRG in the Thai healthcare system, and the NHSO's intention to share know-how with any developing countries that plan to establish universal healthcare coverage.
What is DRG?
Dr. Jadej: DRG is inpatient prospective payment system that categorizes hospitalization costs and determines how much to pay.
Traditionally, physicians and health providers charge patients on a case-by-case basis. Consequently, medical fees are not standardizing, and they can be varied in each patient case.
This challenge led to the invention of DRG, firstly introduced in the United States in 1983, to create a "fair" payment system in which patients and the governments (that run health insurance programs) can identify the sources of medical fees and pay reasonable prices.
How does DRG function in healthcare system?
Dr. Jadej: Let's think about eggs. Hens lay eggs in various sizes. To sell eggs, merchants must group eggs in similar sizes, then assign numbers to them. A group of the largest-sized eggs gets number 1. The smaller ones get number 2, 3, and so on.
We can compare the classification of egg sizes with the principle of DRG. There are more than 40,000 diseases in this world. If health providers charge patients base on the care of each illness, the medical bills of each patient will load with lists of numerous items.
To pay hospitals under this circumstance, the government staff must work on identifying the items in each medical bill, which is very time-consuming and costly.
This problem is solved by DRG payment system. Like grouping eggs by their sizes, the diseases are grouped base on the average resources required to care for those diseases.
For example, appendectomy and colonoscopy are arranged in the same category because health providers use similar resources to provide the services. For Thailand, a myriad of diseases are categorized into 2,500 groups.
Then DRG weight is assigned for each disease group. The higher the DRG weight, the more resources are required to treat a patient, meaning the more expensive medical fees. Medical cost is determined by multiplying DRG weight by cost per relative weight of disease.
Why is DRG payment system essential to the Thai healthcare system?
Dr. Jadej: DRG is applied in inpatient care reimbursement, to replace cost-based reimbursement that had been used widely in the past.
Before the introduction of DRG, Thai healthcare reimbursement was based on fee-for-service system---a traditional payment model where services healthcare providers are reimbursed on the basis of the number of services they provide.
Fee-for-service system undermines the Thai healthcare system by hiking the cost of health service and administrative works. It also encourages physicians to deliver unnecessary care to maximize their profit.
On the other hands, DRG payment system can control healthcare expenses more efficiently, and make sure that Thai healthcare schemes will not go bankrupt by unnecessary medical costs.
How could Thailand succeed in developing DRG model?
Dr. Jadej: During a period of Thai healthcare reform more than two decades ago, we thought about adopting DRG model from the United States. But we needed to buy the model license from an American company, which was unaffordable for us at the time.
Fortunately, Thailand had many talented health researchers. A group of researchers led by Dr. Supasit Pannarunothai took an initiate in developing and modifying Thai-version DRG since the early 1990s, with supports from Health Systems Research Institute and the NHSO.
The UCS, cover health benefit for 49 million Thais, was the first of the Thai health benefit schemes to adopt DRG for inpatient services in 2003. The government's other two healthcare schemes, Social Security Scheme and Civil Servant Medical Benefit Scheme followed in the late 2000s.
The process of DRG development needs participation from health providers. Therefore, we must hold discussions with hospital representatives each year to get their feedback and update the disease classification.
What is the latest progress of Thai DRG?
Dr. Jadej: We have received some good feedback from international organizations, including the World Bank Group that encourages Thailand to take the lead in DRG development for ASEAN countries.
Recently, the Philippines and Vietnam have approached us and shown their interest in using Thai-version DRG. They are at the beginning stage of introducing universal healthcare coverage to their populations, so they need to reform their health financing.
We're aware that DRG is a financial method necessary for starting universal healthcare coverage in developing countries. We are willing to share our resources and our Thai-version DRG without charging any intellectual property fees. We want to be a part of the global effort to achieve universal healthcare coverage in the coming years.
VIDEOS
Thailand's UHC Journey
UHC Public relations