
- Home
- DescriptionNews
A Roi Et hospital endeavors for equitable cervical cancer screening

A Roi Et hospital endeavors for equitable cervical cancer screening
Cancer is a silent health threat with complex causes. But that's not the case for cervical cancer.
Its root cause has been identified as the human papillomavirus (HPV) — leading to the implementation of health programs that emphasize effective screening.
Phanom Phrai Hospital in Thailand’s northeastern Roi Et province has been standing out in proactive efforts to improve the accessibility and equity of cervical cancer screening among women.
In 2022, the province recorded the highest number of cervical cancer screenings in the country, with 40,000 screenings conducted.

Dr Watchara Iamsatsamikul, the Director of Phanom Phrai Hospital, said that the effort to accelerated cervical cancer screening was started 22 years ago when the disease was a leading cause of death among Thai women with cancer, a status that remains unchanged.
In response to this threat, a research team from Chulalongkorn Hospital embarked on finding effective cancer preventive measures and implementing a pilot program in Roi Et province, covering four districts including Phanom Phrai.
As the HPV vaccine was not available at that time, the measures focused on visual inspection with acetic acid and cryotherapy treatment.
The decades of journey in addressing cervical cancer established a systematic and continuous screening approach with a focus on patient-centered care — leading the Roi Et Provincial Public Health Office to receive the United Nations award for the best public service in 2018.
In May of the same year, the World Health Organization (WHO) announced a global call for action to eliminate cervical cancer. It sets the target to reduce the cancer incidence rate of 13.3 to less than four per 100,000 population by 2030.
This will be achieved through three crucial strategies such as administering the HPV vaccine to at least 90% of girls, ensuring at least 70% of targeted women are screened, and providing high-quality treatment for cervical cancer, with a minimum 90% success rate.
The National Health Security Office (NHSO), which oversees the Universal Coverage Scheme (UCS), promptly responded by adding the HPV vaccine in the scheme’s health benefits package and implementing screening programs nationwide — and Phanom Phrai Hospital has actively led this effort.
Addressing the Issue of shame
To ensure effectiveness in cervical cancer screening, Dr Watchara explained that the screening must cover at least 70% of Thai females aged 30-59.

However, shame and embarrassment often prevent women from seeking screenings at healthcare units where technicians perform sample collections.
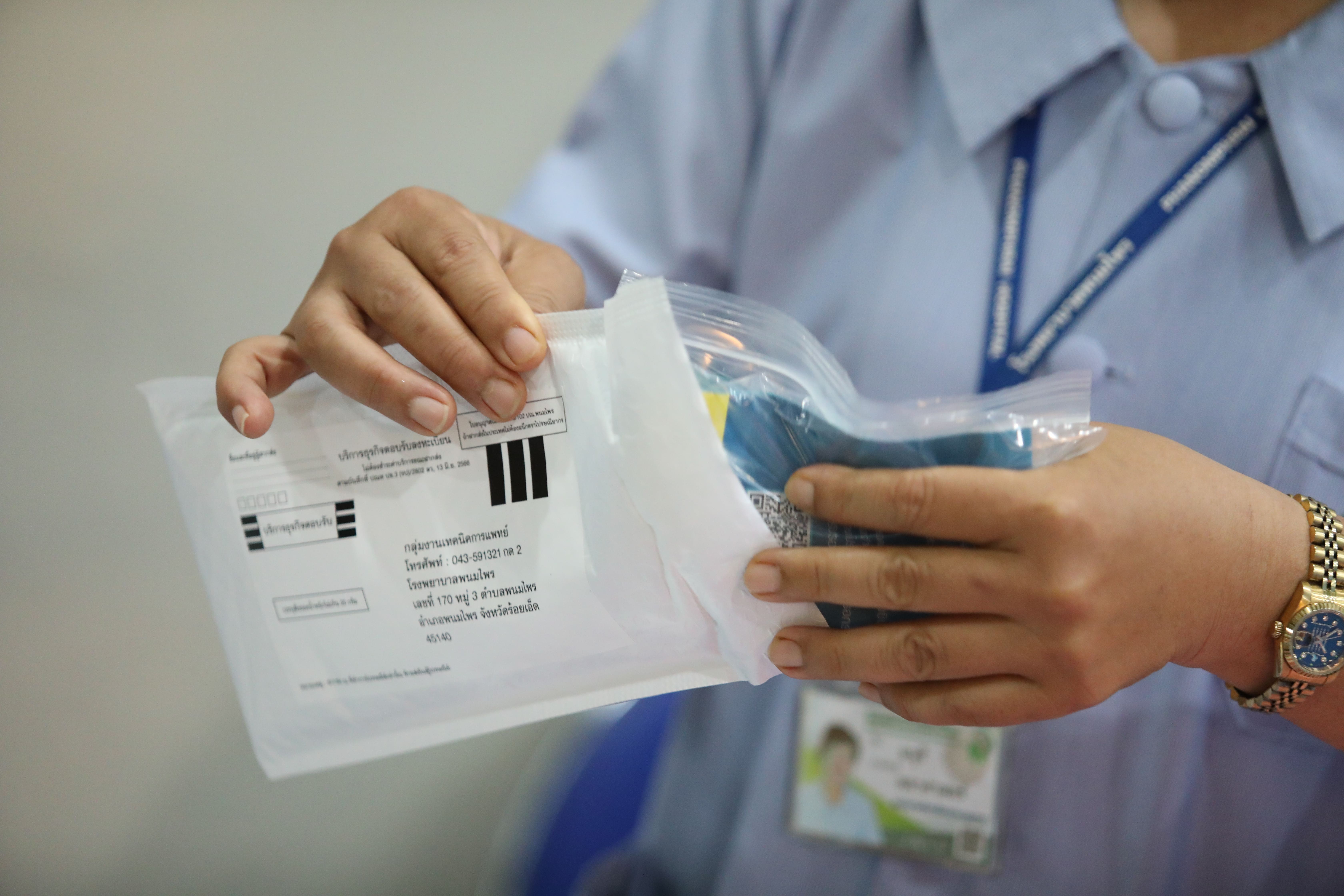
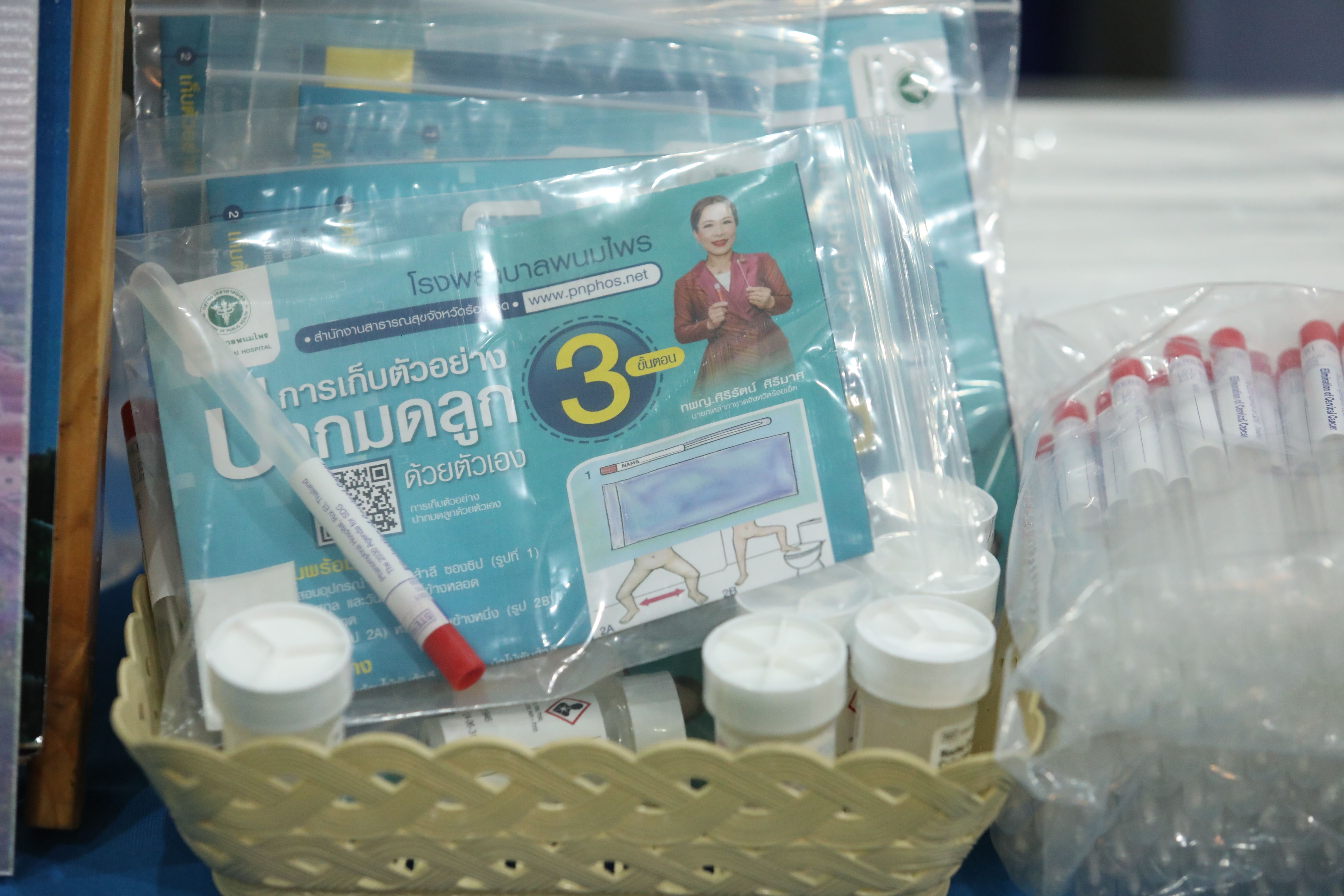
Phanom Phrai Hospital solves this challenge by distributing HPV self-sampling kits. Women can self-collect vaginal samples using the provided devices and send the samples to the hospital.
A study was conducted to compare the accuracy level of the tests using samples collected by healthcare personnel and individuals. It found no significant difference between the two test methods.
This study convinced health authorities to prioritize HPV self-sampling kits and was presented at the conference held by The Royal Thai College of Obstetricians and Gynaecologists.
As a result of these endeavors to expand the screening, the Regional Health Promotion Center 7 Khonkaen is preparing to adopt Phanom Phrai Hospital’s approach throughout part of the northeastern region.
“The current challenge is not about the availability of cervical cancer screening as it is now included in the government’s healthcare care schemes. It’s more about ensuring accessibility for the target groups,” said Dr Watchara.
To reach out to women groups, the hospital staff divided the local population into three segments such as 1) those with registered addresses in Phanom Phrai and residing at home, 2) those with registered addresses but nigrating out, and 3) those without registered addresses but living in the district.
The focus is given to the first and third groups as they can be contacted while finding a strategy to address the second group.
One of the strategies is to involve village health volunteers, who are assigned to contact and follow the people migrating outside the district.
However, most of them declined to receive HPV self-sampling kits — claiming they have full-day work commitments, no fixed address for kit deliveries, or are not able to send the samples back.
Dr Watchara said that more work needs to be done to encourage this group to participate in the screening.
Aggressive outreach program
Following the principle of leaving no one behind, Phanom Phrai Hospital has implemented an aggressive outreach health program to enable more women to access cervical cancer screening.
The program includes visiting workplaces to distribute HPV self-sampling kits to the workers.
Upon implementing this program at one factory with over 2,500 employees, the hospital staff found 1,200 women within the age criteria for the screening. But only 8.9% of them previously underwent the tests.
Around 370 self-collection kits were handed to these workers, with an 80% return rate. The test results found that 9% of the samples indicated the risk of cervical cancer, double the risk detection rate among women having screenings at the point of healthcare entry.
The hospital staff has also distributed HPV self-sampling kits to partnered clinics and pharmacies, where female customers receive the devices.
Phanom Phrai Hospital set up a medical laboratory, becoming the second such facility in Roi Et province, to accommodate the increasing number of tests.
“Cervical cancer screening not only promotes health equity but also addresses health disparity,” said Dr Watchara.
“It is not just a general health issue, but it disproportionately affects marginalized populations, with a ratio of 80:20 of people having the disease between impoverished and affluent countries. Investing in comprehensive disease screening is a way to diminish health inequalities for everyone.”

