
- Home
- DescriptionNews
Community-based isolation: a solution for managing healthcare strain.

Community-based isolation: a solution for managing healthcare strain.
With rising COVID-19 new cases, Bangkok metropolitan region is declared a pandemic hotspot by the Thai government.
Two by three of nearly 10,000 new daily cases reported in Thailand are concentrated in the region. The influx of patients at hospitals exhausts medical professionals and health workers. Bed occupancy is brimful. Patients wait longer to get beds. Some of them die while staying at home, unable to obtain hospital care.
We genuinely feel sorry about their loss and feel the suffering of people who must observe the illness and death in the last one and a half years.
But we also believe that there is hope at the end of the tunnel. We see the solidarity of people who put in great effort to help and comfort others. Many come up with solutions to fill the gap in the health system.
One of the solutions that we recognize is the collaboration among multi-stakeholders in Bangkok to initiate "Home Isolation" and "Community Isolation" programs.
This program involves individuals, local communities, civil society groups, and hospital operators to provide care and assistance to COVID-19 patients with mild symptoms. It helps patients reach out to physicians or medical staff via video calls, medical devices, and medicine delivery services.
The program does not just help prevent the spread of the coronavirus, especially in a household with several members living together in a crowded space. It also helps to reducing the crowd at hospitals, allowing medical staff to focus on critical cases.
This idea does not come out of the blue. It is based on data and the communities' observation on the high prevalence of mild-symptom patients among those tested positive.
As of June 4, around 19,430 hospital beds in Bangkok metropolitan region were occupied by COVID-19 patients. Only 65 of those were critical cases. The bed occupancy increased to more than 29,000 in early July, with around 1,140 severe cases, after the highly contagious Delta variant spread throughout the region.
These numbers show that hospital beds are mainly occupied by mild-symptom patients, many of which are not required hospital admissions. They can recover at home if they get to rest and take medicines properly. In addition, health experts found that the ratio of patients with mild, moderate, and severe symptoms is at 80: 15: 5.
Aware of this data, Rajavithi Hospital, for example, piloted home isolation care for 18 patients last month. Doctors closely monitored them via video calls. Hospital staff delivered medicines and meals to their home every day. Most of them recover now, proving that home isolation is possible and effective if we can ensure a good monitoring system.
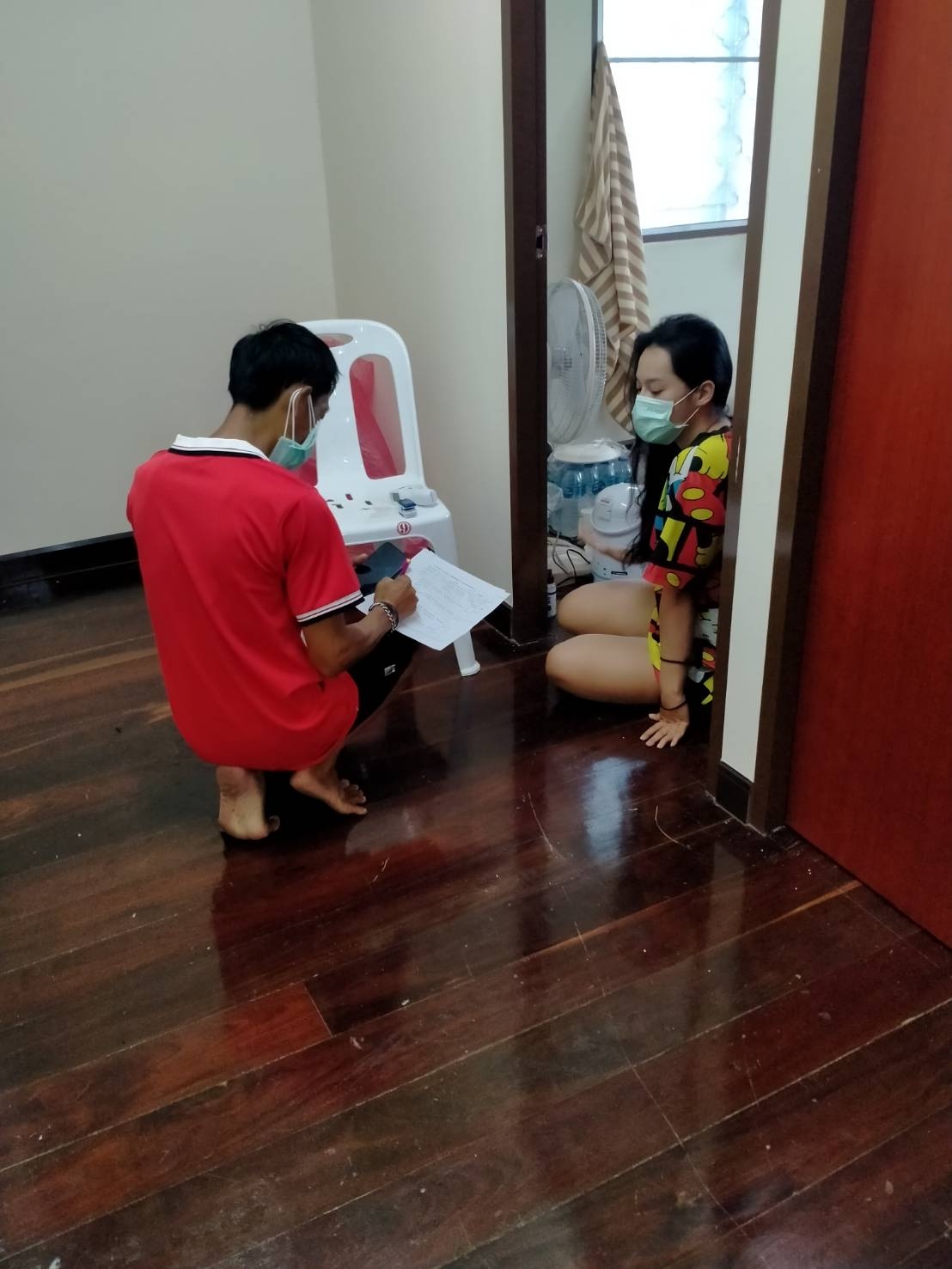
On the other hand, community isolation is a collective approach in which local communities turn communal buildings such as temples and community halls into isolation facilities.
Institute of HIV Research and Innovation (IHRI) is a frontline organization that helps many local communities in Bangkok manage the facilities and set up a patient monitoring system, in collaboration with non-governmental organizations such as Human Settlement Foundation and Duang Prateep Foundation.
IHRI staff has trained community leaders to search high-risk persons, distinguish the severity levels of COVID-19 patients, and provide the proper care to them. Equip with knowledge, each community leader formed a COVID-19 working group and transferred that knowledge to the group members.
IHRI team also connected this working group with medical staff at Piyavate Hospital, of which staff dispatched mobile X-ray vehicles and medicines to the communities. Physicians from the hospital arrange video conferences with patients once every three days.
If their conditions worsen, hospital staff will send ambulances to pick them up and transfer them to a hospital facility to get intensive care.
Community isolation is a bottom-up solution that empowers local communities to fight the pandemic while ensuring healthcare access for COVID-19 patients under tight healthcare resources.
Its success is recognized by Public Health Ministry, the NHSO, and Bangkok Metropolitan Administration and adopted at the policy level.
From July 12, asymptomatic and mild-symptom patients in Bangkok will be placed into the home or community isolation under close monitoring of medical staff hospitals or community clinics partnering with the NHSO.
There are 204 clinics located across Bangkok. Each can look after 200 patients. Meanwhile, the community isolation model is in progress to expand into 23 communities across the capital.
NHSO will cover expenses of medical services and provisions given to COVID-19 patients under this program---including RT-PCR and rapid antigen test, laboratory service, patient transfer, mobile chest X-ray service, daily meals, medical devices, and personal protective equipment for medical staff.
On behalf of the NHSO, I want to thank all parties involved in creating this community-based solution to fill the gap in Bangkok's health system that serves more than 10 million people.
I want to emphasize that this program does not leave patients to their fate at home. It helps patients get faster access to physicians, treatment, and medicines via virtual consultation and home delivery services. It's much better than leaving patients in uncertainty while waiting days and nights for hospital beds.
In the time of crisis, we see the strength of all stakeholders in the health system. We shall engage them, empower them, and trust them. As long as we collaborate, we should be able to get through the crisis together.
Dr Jadej Thammathach-Aree
Secretary-General of National Health Security Office (NHSO)
14 July 2021

