
- Home
- DescriptionNews
NHSO continues to thrive as approaching the 20th year
NHSO continues to thrive as approaching the 20th year
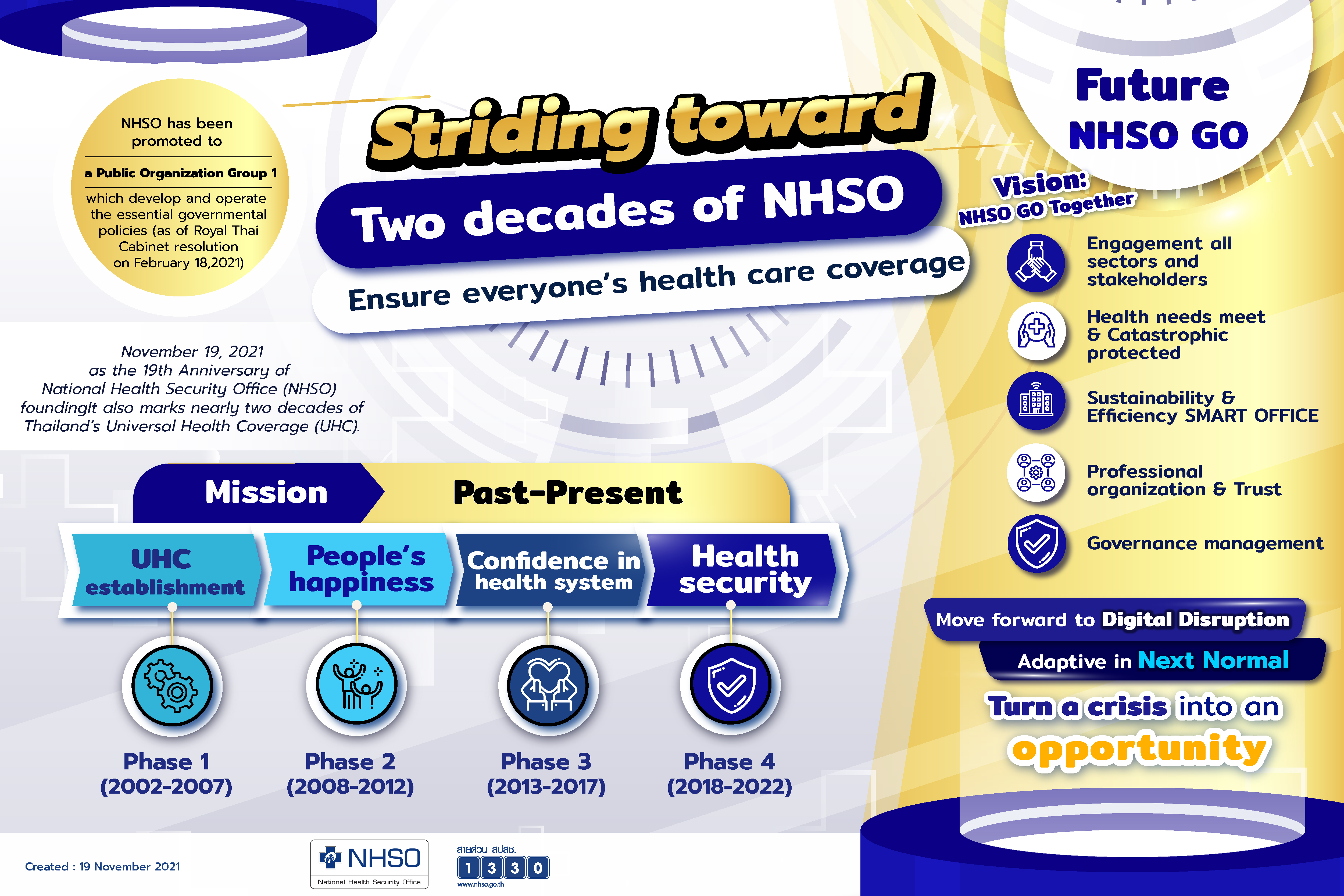
Looking back at the past 19 years since its establishment, the National Health Security Office (NHSO) has seen itself overcoming numerous challenges and achieving various goals in operating the Universal Coverage Scheme (UCS).
Now that it is heading into the 20th year of its operations, the NHSO is still committed to continuing improving public access to necessary healthcare services under the UCS so that no one won’t end up becoming financially insecure as a result high-cost treatments.
.jpg)
This ultimate goal of the NHSO in operating the UCS remained firm over the past 19 years and will continue to be in the years to come, said Dr Jadej Thammatacharee, secretary-general of the NHSO, marking the 19th anniversary of the NHSO on Nov 19, 2021.
Improvement in public access to healthcare under the UCS has been continuing in the past 19 years, during which financial burdens facing patients and their families have dramatically been eased, he said.
Aside from the NHSO’s determination and commitment to improve the public access to healthcare services, its willingness to listen to opinions from all parties and compile them into new policies in operating the UCS really is the key to success.
“The past success, however, doesn’t guarantee more success as there still are more challenges lying ahead for the NHSO to deal with and weak points to fix in order to achieve even more success,” he said.
In order to succeed more in further developing the healthcare system in the next few years, the NHSO will probably have to adopt a paradigm shift in the way it works, he said.
The NHSO secretary-general himself is determined to focus mainly on two theories he has recently adopted for improving his way of working, namely “behavioral economics” and “the world in a disruptive era”.
Some examples of the preliminary outcome of applying these theories to the work of the NHSO include having medications delivered to certain types of patients at their homes, making it possible for a number of patients to be discharged from the hospital the following day after they undergo an operation and supporting certain cancer patients to receive treatment at home, said Dr Jadej.
Previously, a principle behind these new healthcare programmes – getting as more patients to receive healthcare while at the same time shortening the time healthcare providers work to serve them -- appeared to be nearly impossible, he said.
Now that the NHSO has proved it can make the impossible possible, more of such healthcare innovations will follow, he said.
And as the world is being disrupted by new technologies, he said, the NHSO has proved that sometimes an expensive new technology isn’t necessarily better.
The NHSO’s home isolation programme for COVID-19 infected patients, costing about 10,000 baht per person, has eventually become even more popular among the patients than the hotel isolation programme offered by a number of hotels at a cost of about 60,000 baht per person, he said.
The reason is many infected patients tend to feel more comfortable with staying home during COVID-19 isolation, in which they are provided with necessary medications and medical devices right at their homes, than to stay at a hotel during such isolation, he said.
“This has reflected the truth that a lower-cost service isn’t necessarily a worse choice while costlier technologies aren’t always better,” he said.
The NHSO secretary-general has also underlined the importance of a speedy response to the need to deal with a new work challenge, which has been proven to be a key factor in the NHSO’s past successes in the past 19 years, he said.
The no-fault compensation programme for the people suffering an adverse event following COVID-19 vaccination is an example of the NHSO’s fast action that has led to a fast success, he said.
“We’ve aimed to get the financial compensation done as fast as in five days, which aren’t five working days. If commercial banks can handle transactions on also Saturdays and Sundays, so can we,” he said.

In an outsider’s point of view, the continuous improvement of healthcare benefits offered under the UCS has greatly benefited many patients and consequently raised confidence among them in the standard of healthcare provided under the scheme, said Sirintip Kudtiyakarn, chairwoman of Thai Cancer Society (TCS).
In a common opinion shared among the cancer patients receiving treatment under the UCS, that the UCS now offers cancer care and treatment as equally good as one offered under the other healthcare schemes, she said.
“Treating cancer is a race against time, which is complicated and costly. And the disease affects not only the patients themselves but also their families,” she said. “Since many of these patients haven’t before prepared for high treatment costs, the UCS does help save them [from a possible financial crisis].”
As for a suggestion from the TCS, she said, the UCS’ core benefit package should also include screening for common types of cancer such as breast cancer and liver cancer.
More attention should also be paid to improving the quality of life of cancer patients by allowing them to choose treatment and care options they may find more favourable to them, she said.
And if possible, cancer patients should also be allowed to have a role in the decision-making process of the UCS’ development of its cancer care programme and patient networking, not only taking part in certain activities organised by the NHSO, she said.
Last but not least, she said, the system for sharing the data of cancer patients and their treatments under the UCS’ cancer treatment programme between state-run cancer-treating institutions and their private-run counterparts can still be improved to achieve seamless connection, she said.
When merged into one whole database system of cancer patients and treatment, the system will serve as an important source of information for future policy making and budgetary management, she said.
///

